
IT’S ALL ABOUT SEX
A tiny sperm from dad breaks through the surface of a huge egg from mom. Voilà! In nine months, a new son or daughter will be born. Like most other multicellular organisms, human beings reproduce sexually. In human sexual reproduction, males produce sperm and females produce eggs, and a new offspring forms when a sperm unites with an egg. How do sperm and eggs form? And how do they arrive together at the right place and time so they can unite to form a new offspring? These are functions of the reproductive system.
WHAT IS THE REPRODUCTIVE SYSTEM?
The reproductive system is the human organ system responsible for the production and fertilization of gametes (sperm or eggs) and, in females, the carrying of a fetus. Both male and female reproductive systems have organs called gonads that produce gametes. A gamete is a haploid cell that combines with another haploid gamete during fertilization, forming a single diploid cell called a zygote. Besides producing gametes, the gonads also produce sex hormones. Sex hormones are endocrine hormones that control the development of sex organs before birth, sexual maturation at puberty, and reproduction once sexual maturation has occurred. Other reproductive system organs have various functions, such as maturing gametes, delivering gametes to the site of fertilization, and providing an environment for the development and growth of an offspring.
SEX DIFFERENTIATION
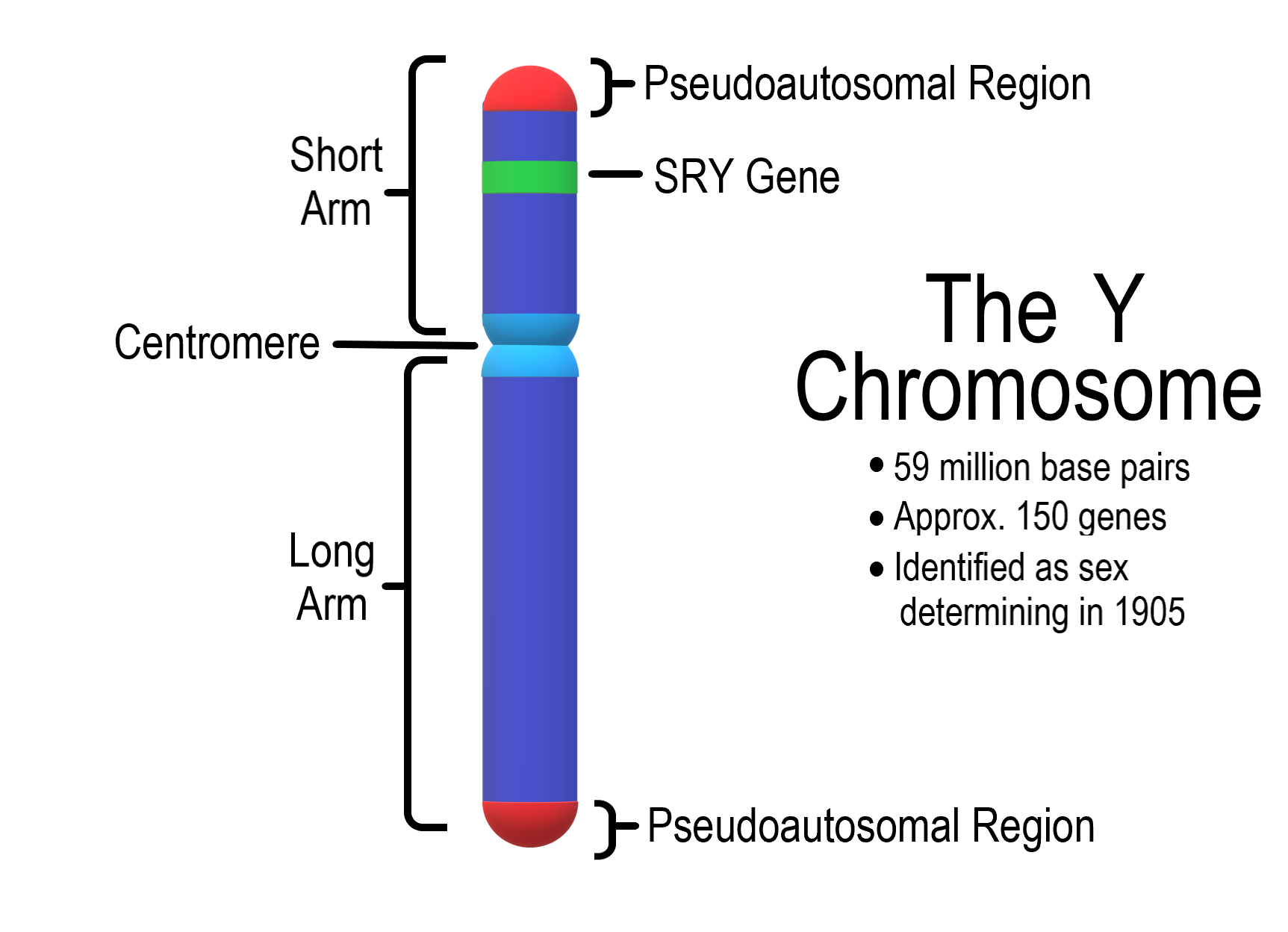
Starting around the seventh week after conception in genetically male (XY) embryos, a gene called SRY on the Y chromosome (shown in Figure 14.2) initiates the production of multiple proteins. These proteins cause undifferentiated gonadal tissue to develop into male gonads (testes). The male gonads then secrete hormones — including the male sex hormone testosterone — that trigger other changes in the developing offspring (now called a fetus), causing it to develop a complete male reproductive system. Without a Y chromosome, an embryo will develop female gonads (ovaries) that will produce the female sex hormone estrogen. Estrogen, in turn, will lead to the formation of the other organs of a normal female reproductive system.
HOMOLOGOUS STRUCTURES
Undifferentiated embryonic tissues develop into different structures in male and female fetuses. Structures that arise from the same tissues in males and females are called homologous structures. The male testes and female ovaries, for example, are homologous structures that develop from the undifferentiated gonads of the embryo. Likewise, the male penis and female clitoris are homologous structures that develop from the same embryonic tissues.
SEX HORMONES AND MATURATION
Male and female reproductive systems are different at birth, but they are immature and incapable of producing gametes or sex hormones. Maturation of the reproductive system occurs during puberty, when hormones from the hypothalamus and pituitary gland stimulate the testes or ovaries to start producing sex hormones again. The main sex hormones are testosterone in males and estrogen in females. Sex hormones, in turn, lead to the growth and maturation of the reproductive organs, rapid body growth, and the development of secondary sex characteristics. Secondary sex characteristics are traits that are different in mature males and females but are not directly involved in reproduction. They include facial hair in males and breasts in females.
Review
- What are gonads?
- What are sex hormones?
- Give an example of a secondary sex characteristic.
14.3 MALE REPRODUCTIVE SYSTEM
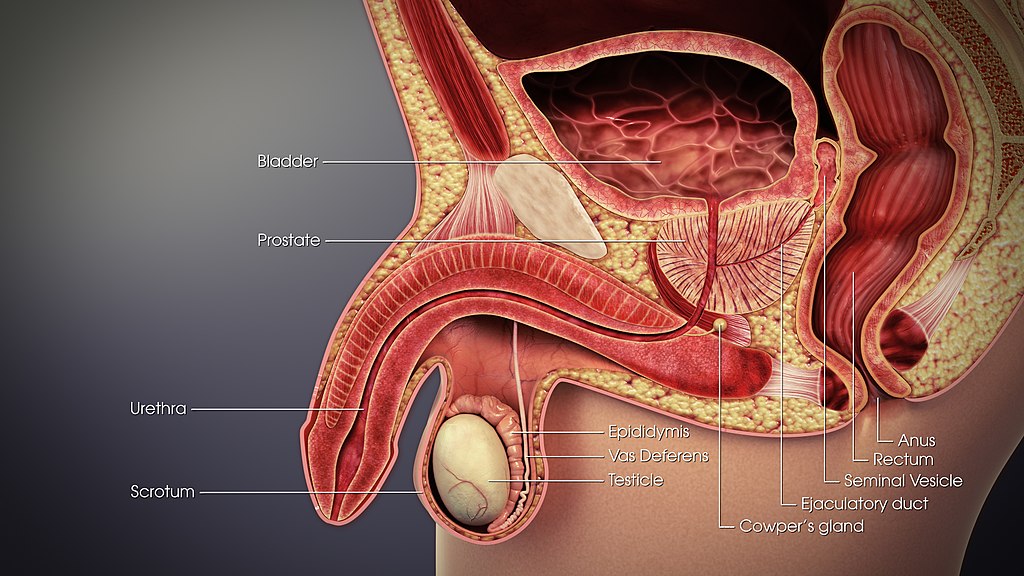
The main structures of the male reproductive system are external to the body and illustrated in Figure 14.3. The two testes (singular, testis) hang between the thighs in a sac of skin called the scrotum. The scrotum is a pouch of skin and smooth muscle that hangs down behind the penis. Its function is to control the temperature of the testes. The testes produce both sperm and testosterone. Resting atop each testis is a coiled structure called the epididymis (plural, epididymes). The function of the epididymes is to mature and store sperm. The penis is a tubular organ that contains the urethra and has the ability to stiffen during sexual arousal. Sperm passes out of the body through the urethra during a sexual climax (orgasm). This release of sperm is called ejaculation.
In addition to these organs, the male reproductive system consists of several ducts and glands that are internal to the body. The ducts, which include the vas deferens (also called the ductus deferens), transport sperm from the epididymis to the urethra. The glands, which include the prostate gland and seminal vesicles, produce fluids that become part of semen. Semen is the fluid that carries sperm through the urethra and out of the body. It contains substances that control pH and provide sperm with nutrients for energy.
TESTES STRUCTURE
The testes are filled with hundreds of tiny tubes, called seminiferous tubules, which are the functional units of the testes. As shown in the longitudinal section drawing of a testis in Figure 14.4, the seminiferous tubules are coiled and tightly packed within divisions of the testis called lobules. Lobules are separated from one another by internal walls (or septa).
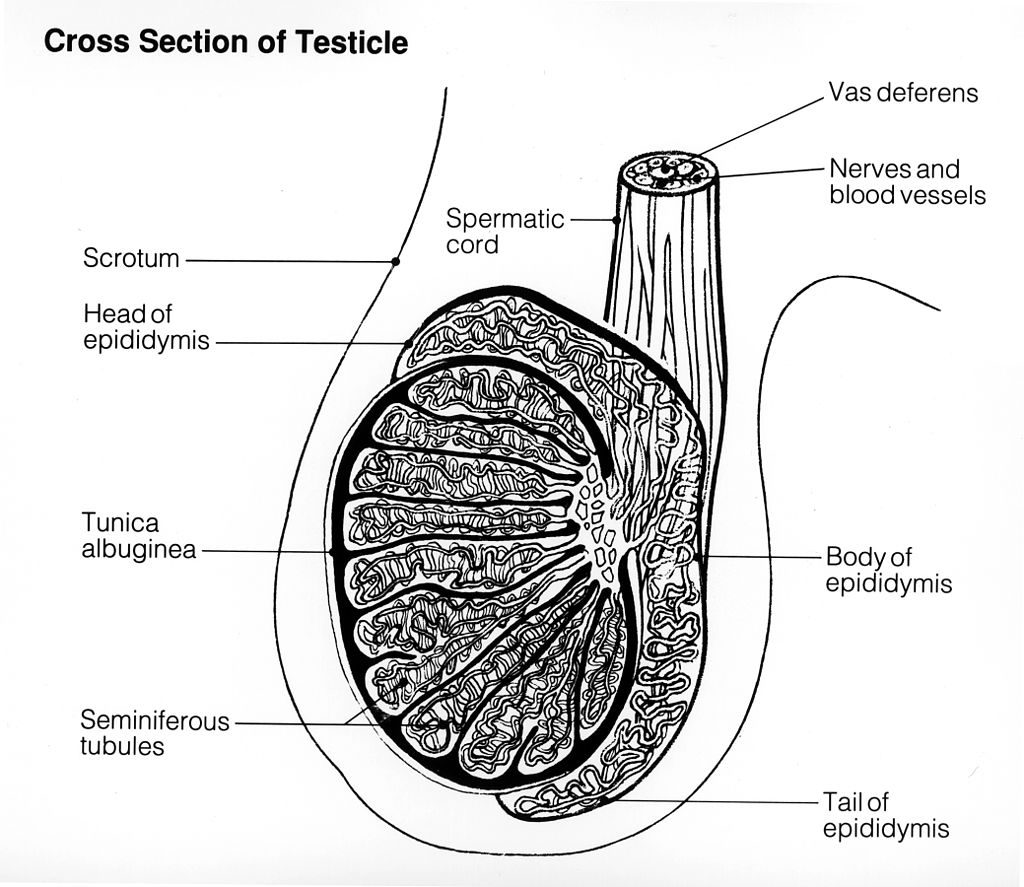
Figure 14.4 This longitudinal-section drawing includes a testis on the left, its corresponding epididymis in the center, and its related vas (or ductus) deferens on the right. The three structures are connected to create a tract through which sperm can travel.
Seminiferous Tubules
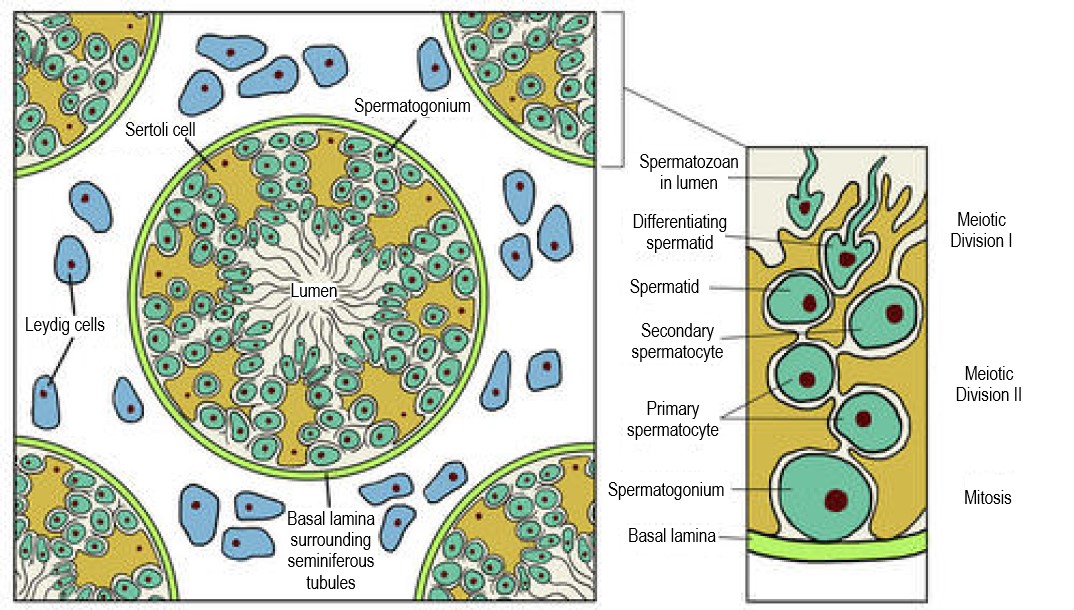
One or more seminiferous tubules are tightly coiled within each of the hundreds of lobules in the testis. A single testis normally contains a total of about 30 meters of these tightly packed tubules! As shown in the cross-sectional drawing of a seminiferous tubule in Figure 14.5, the tubule contains sperm in several different stages of development (spermatogonia, spermatocytes, spermatids, and spermatozoa). The seminiferous tubule is also lined with epithelial cells called Sertoli cells. These cells release a hormone (inhibin) that helps regulate sperm production. Adjacent Sertoli cells are closely spaced so large molecules cannot pass from the blood into the tubules. This prevents the male’s immune system from reacting against the developing sperm, which may be antigenically different from his own self tissues. Cells of another type, called Leydig cells, also known as Interstitial cells, are found between the seminiferous tubules. Leydig cells produce and secrete testosterone.
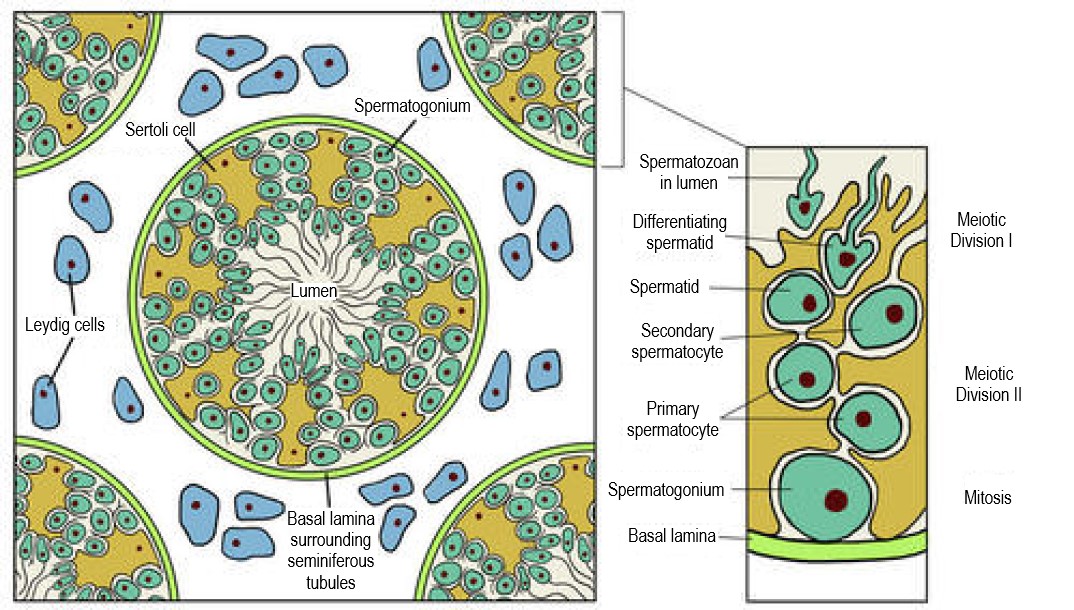
Figure 14.5 A cross-sectional drawing of a testis and seminiferous tubule shows the lining of Sertoli cells and sperm in different stages of development within the tubule, and Leydig cells surrounding the tubule.
Besides the two testes, the scrotum also contains a pair of organs called epididymes (singular, epididymis) and part of each of the paired vas deferens (or ducti deferens). Both structures play important functions in the production or transport of sperm.
Epididymis
The seminiferous tubules within each testis join together to form ducts (called efferent ducts) that transport immature sperm to the epididymis associated with that testis. Each epididymis (plural, epididymes) consists of a tightly coiled tubule with a total length of about 6 meters. As shown in Figure 14.6, the epididymis is generally divided into three parts: the head (which rests on top of the testis), the body (which drapes down the side of the testis), and the tail (which joins with the vas deferens near the bottom of the testis). The functions of the two epididymes are to mature sperm, and then to store that mature sperm until they leave the body during an ejaculation, when they pass the sperm on to the vas deferens.
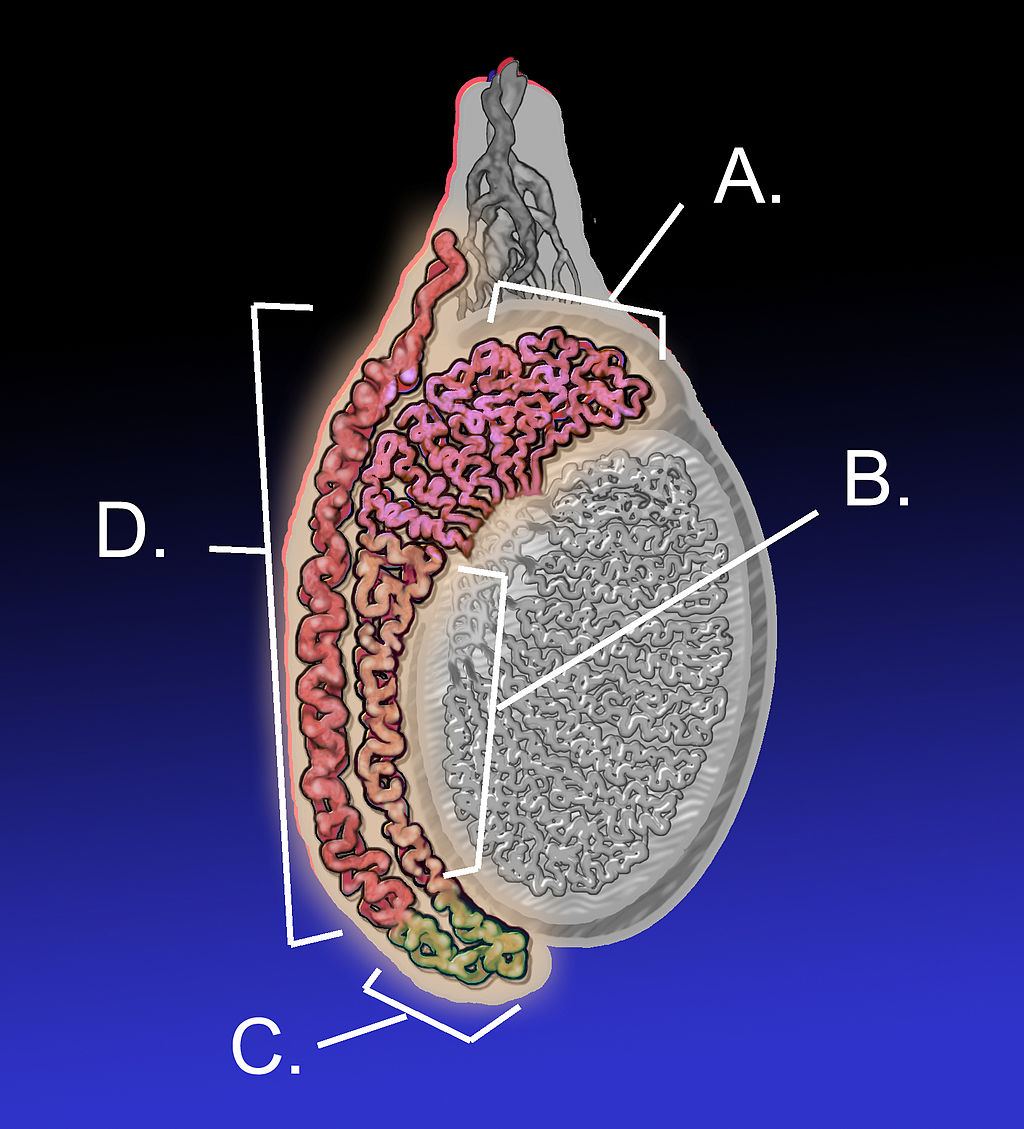
Figure 14.6 Each epididymis consists of a (a) head, (b) body, and (c) tail. The latter is directly connected to the (d) vas deferens. The gray egg-shaped structure in the drawing is the testis.
Vas Deferens
The vas deferens, also known as sperm ducts or ductus deferens, are a pair of thin tubes, each about 30 cm (almost 12 in) long, which begin at the epididymes in the scrotum, and continue up into the pelvic cavity. They are composed of ciliated epithelium and smooth muscle. These structures help the vas deferens fulfill their function of transporting sperm from the epididymes to the ejaculatory ducts, which are accessory structures of the male reproductive system.
ACCESSORY STRUCTURES
In addition to the structures within the scrotum, the male reproductive system includes several internal accessory structures that are shown in the detailed drawing in Figure 14.3. They include the ejaculatory ducts, seminal vesicles, and the prostate and bulbourethral (Cowper’s) glands.
SEMINAL VESICLES
The seminal vesicles are a pair of exocrine glands that each consist of a single tube, which is folded and coiled upon itself. Each vesicle is about 5 cm (almost 2 in) long and has an excretory duct that merges with the vas deferens to form one of the two ejaculatory ducts. Fluid secreted by the seminal vesicles into the ducts makes up about 70% of the total volume of semen, which is the sperm-containing fluid that leaves the penis during an ejaculation. The fluid from the seminal vesicles is alkaline, so it gives semen a basic pH that helps prolong the lifespan of sperm after it enters the acidic secretions inside the female vagina. Fluid from the seminal vesicles also contains proteins, fructose (a simple sugar), and other substances that help nourish sperm.
EJACULATORY DUCTS
The ejaculatory ducts form where the vas deferens join with the ducts of the seminal vesicles in the prostate gland. They connect the vas deferens with the urethra. The ejaculatory ducts carry sperm from the vas deferens, as well as secretions from the seminal vesicles and prostate gland that together form semen. The substances secreted into semen by the glands as it passes through the ejaculatory ducts control its pH and provide nutrients to sperm, among other functions. The fluid itself provides sperm with a medium in which to “swim.”
PROSTATE GLAND
The prostate gland is located just below the seminal vesicles. It is a walnut-sized organ that surrounds the urethra and its junction with the two ejaculatory ducts. The function of the prostate gland is to secrete a slightly alkaline fluid that constitutes close to 30% of the total volume of semen. Prostate fluid contains small quantities of proteins, such as enzymes. In addition, it has a very high concentration of zinc, which is an important nutrient for maintaining sperm quality and motility.
BULBOURETHRAL GLANDS
Also called Cowper’s glands, the two bulbourethral glands are each about the size of a pea and located just below the prostate gland. The bulbourethral glands secrete a clear, alkaline fluid that is rich in proteins. Each of the glands has a short duct that carries the secretions into the urethra, where they make up a tiny percentage of the total volume of semen. The function of the bulbourethral secretions is to help lubricate the urethra and neutralize any urine (which is acidic) that may remain in the urethra.
PENIS
The penis is the external male organ that has the reproductive function of delivering sperm to the female reproductive tract. This function is called intromission. The penis also serves as the organ that excretes urine.
STRUCTURE OF THE PENIS
The structure of the penis and its location relative to other reproductive organs are shown in Figure 14.7. The part of the penis that is located inside the body and out of sight is called the root of the penis. The shaft of the penis is the part of the penis that is outside the body. The enlarged, bulbous end of the shaft is called the glans penis.
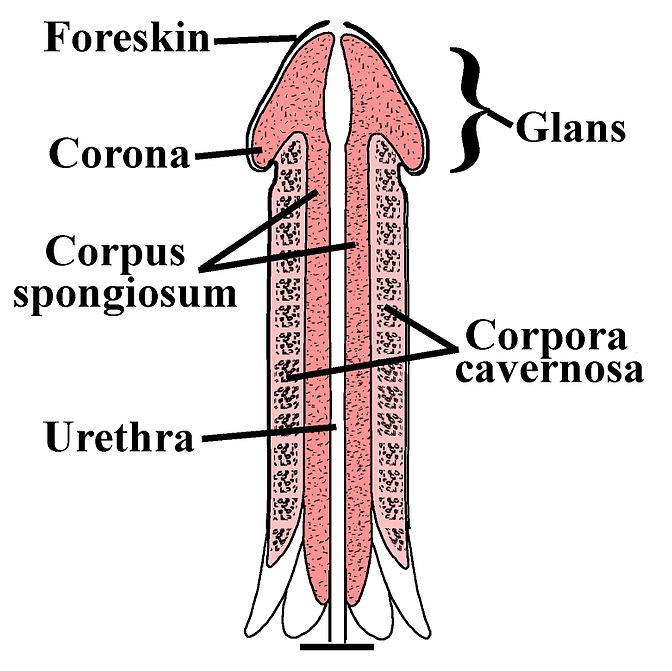
URETHRA
The urethra passes through the penis to carry urine from the bladder — or semen from the ejaculatory ducts — through the penis and out of the body. After leaving the urinary bladder, the urethra passes through the prostate gland, where the urethra is joined by the ejaculatory ducts. From there, the urethra passes through the penis to its external opening at the tip of the glans penis. Called the external urethral orifice, this opening provides a way for urine or semen to leave the body.
Review
- Describe the structure of a testis.
- Which parts of the male reproductive system are connected by the ejaculatory ducts? What fluids enter and leave the ejaculatory ducts?
- A vasectomy is a form of birth control for men that is performed by surgically cutting or blocking the vas deferens so that sperm cannot be ejaculated out of the body. Do you think men who have a vasectomy emit semen when they ejaculate? Why or why not?
- What are the three accessory organs of the male reproductive system and what is the function of each?
- What are the seminiferous tubules?
- What cells produce testosterone?
- What is the function of the epididymis?
- What path do sperm take to exit the male reproductive system?
14.4 FUNCTIONS OF THE MALE REPRODUCTIVE SYSTEM
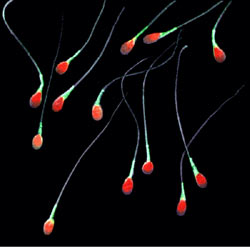
COLORFUL SPERM
This false-color image (Figure 14.8) shows real human sperm. The tiny gametes are obviously greatly magnified in the picture, because they are actually the smallest of all human cells. In fact, human sperm cells are small, even when compared with sperm cells of other animals. Mice sperm are about twice the length of human sperm! Human sperm may be small in size, but in a normal, healthy man, huge numbers of them are usually released during each ejaculation. There may be hundreds of millions of sperm cells in a single teaspoon of semen. Producing sperm is one of the major functions of the male reproductive system.
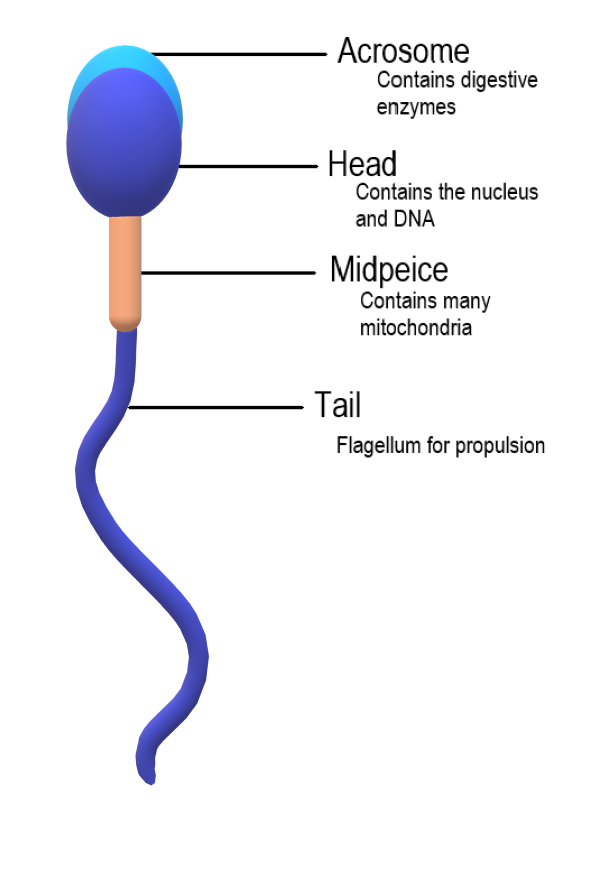
SPERM ANATOMY
A mature sperm cell has several structures that help it reach and penetrate an egg. These are labeled in the drawing of a sperm shown in Figure 14.9.
- The head is the part of the sperm that contains the nucleus — and not much else. The nucleus, in turn, contains tightly coiled DNA that is the male parent’s contribution to the genetic makeup of a zygote (if one forms). Each sperm is a haploid cell, containing half the chromosomal complement of a normal, diploid body cell.
- The front of the head is an area called the acrosome. The acrosome contains enzymes that help the sperm penetrate an ovum (if it reaches one).
- The midpiece is the part of the sperm between the head and the flagellum. The midpiece is packed with mitochondria that produce the energy needed to move the flagellum.
- The flagellum (also called the tail) can rotate like a propeller, allowing the sperm to “swim” through the female reproductive tract to reach an ovum if one is present.
SPERMATOGENESIS
The process of producing sperm is known as spermatogenesis. Spermatogenesis normally starts when a male reaches puberty, and it usually continues uninterrupted until death, although a decrease in sperm production generally occurs at older ages. A young, healthy male may produce hundreds of millions of sperm a day! Only about half of these, however, are likely to become viable, mature sperm.
WHERE SPERM ARE PRODUCED
Spermatogenesis occurs in the seminiferous tubules in the testes. Spermatogenesis requires high concentrations of testosterone. Testosterone is secreted by Leydig cells, which are adjacent to the seminiferous tubules in the testes.
Sperm production in the seminiferous tubules is very sensitive to temperature. This may be the most important reason the testes are located outside the body in the scrotum. The temperature inside the scrotum is generally about 2 degrees Celsius cooler than core body temperature. This lower temperature is optimal for spermatogenesis. The scrotum regulates its internal temperature as needed by contractions of the smooth muscles lining the scrotum. When the temperature inside the scrotum becomes too low, the scrotal muscles contract. The contraction of the muscles pulls the scrotum higher against the body, where the temperature is warmer. The opposite occurs when the temperature inside the scrotum becomes too high.
EVENTS OF SPERMATOGENESIS
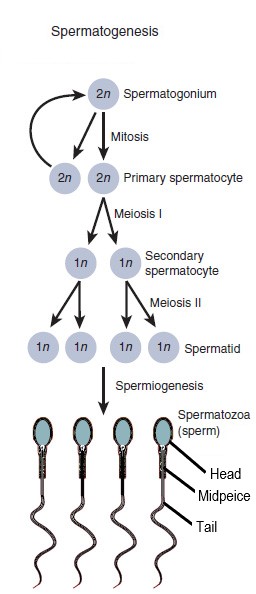
Figure 14.10 summarizes the main cellular events that occur in the process of spermatogenesis. The process begins with a diploid stem cell called a spermatogonium (plural, spermatogonia), and involves several cell divisions. The entire process takes at least ten weeks to complete, including maturation in the epididymis.
- A spermatogonium undergoes mitosis to produce two diploid cells called primary spermatocytes. One of the primary spermatocytes goes on to produce sperm. The other replenishes the reserve of spermatogonia.
- The primary spermatocyte undergoes meiosis I to produce two haploid daughter cells called secondary spermatocytes.
- The secondary spermatocytes rapidly undergo meiosis II to produce a total of four haploid daughter cells called spermatids.
- The spermatids begin to form a tail, and their DNA becomes highly condensed. Unnecessary cytoplasm and organelles are removed from the cells, and they form a head, midpiece, and flagellum. The resulting cells are sperm (spermatozoa).
As shown in Figure 14.11, the events of spermatogenesis begin near the wall of the seminiferous tubule — where spermatogonia are located — and continue inward toward the lumen of the tubule. Sertoli cells extend from the wall of the seminiferous tubule inward toward the lumen, so they are in contact with developing sperm at all stages of spermatogenesis. Sertoli cells play several roles in spermatogenesis:
- They secrete endocrine hormones that help regulate spermatogenesis.
- They secrete substances that initiate meiosis .
- They concentrate testosterone (from Leydig cells), which is needed at high levels to maintain spermatogenesis.
- They phagocytize the extra cytoplasm that is shed from developing sperm cells.
- They secrete testicular fluid that helps carry sperm into the epididymis.
- They maintain a blood-testis barrier, so immune system cells cannot reach and attack the sperm.
Human Physiology – Reproduction: Spermatogenesis, Janux, 2015.
MATURATION IN THE EPIDIDYMIS
Although the sperm produced in the testes have tails, they are not yet motile (able to “swim”). The non-motile sperm are transported to the epididymis in testicular fluid that is secreted by Sertoli cells with the help of peristaltic contractions. In the epididymis, the sperm gain motility, so they are capable of swimming up the female genital tract and reaching an ovum. The mature sperm are stored in the epididymis until ejaculation occurs.
EJACULATION
Sperm are released from the body during ejaculation, which typically occurs during orgasm. Hundreds of millions of mature sperm — contained within a small amount of thick, whitish fluid called semen — are propelled from the penis during a normal ejaculation.
HOW EJACULATION OCCURS
Ejaculation occurs when peristalsis of the muscle layers of the vas deferens and other accessory structures propel sperm from the epididymes, where mature sperm are stored. The muscle contractions force the sperm through the vas deferens and the ejaculatory ducts, and then out of the penis through the urethra. Due to the peristaltic action of the muscles, the ejaculation occurs in a series of spurts.
THE ROLE OF SEMEN
As sperm travel through the ejaculatory ducts during ejaculation, they mix with secretions from the seminal vesicles, prostate gland, and bulbourethral glands to form semen (see Figure 14.12). The average amount of semen per ejaculate is about 3.7 mL, which is a little less than a teaspoonful. Most of this volume of semen consists of glandular secretions, with the hundreds of millions of sperm cells actually contributing relatively little to the total volume.

The secretions in semen are important for the survival and motility of sperm. They provide a medium through which sperm can swim. They also include sperm-sustaining substances, such as high concentrations of the sugar fructose, which is the main source of energy for sperm. In addition, semen contains many alkaline substances that help neutralize the acidic environment in the female vagina. This protects the DNA in sperm from being denatured by acid, and prolongs the life of sperm in the female reproductive tract.
ERECTION
Besides providing a way for sperm to leave the body, the main role of the penis in reproduction is intromission, or depositing sperm in the vagina of the female reproductive tract. Intromission depends on the ability of the penis to become stiff and erect, a state referred to as an erection. The human penis, unlike that of most other mammals, contains no erectile bone. Instead, in order to reach its erect state, it relies entirely on engorgement with blood of its columns of spongy tissue. During sexual arousal, the arteries that supply blood to the penis dilate, allowing more blood to fill the spongy tissue. The now-engorged spongy tissue presses against and constricts the veins that carry blood away from the penis. As a result, more blood enters than leaves the penis, until a constant erectile size is achieved.
In addition to sperm, the penis also transports urine out of the body. These two functions cannot occur simultaneously. During an erection, the sphincters that prevent urine from leaving the bladder are controlled by centers in the brain so they cannot relax and allow urine to enter the urethra.
TESTOSTERONE PRODUCTION
The final major function of the male reproductive system is the production of the male sex hormone testosterone. In mature males, this occurs mainly in the testes. Testosterone production is under the control of luteinizing hormone (LH) from the pituitary gland. LH stimulates Leydig cells in the testes to secrete testosterone.
Testosterone is important for male sexual development at puberty. It stimulates maturation of the male reproductive organs, as well as the development of secondary male sex characteristics (such as facial hair). Testosterone is also needed in mature males for normal spermatogenesis to be maintained in the testes. Follicle stimulating hormone (FSH) from the pituitary gland is also needed for spermatogenesis to occur, in part because it helps Sertoli cells in the testes concentrate testosterone to high enough levels to maintain sperm production. Testosterone is also needed for proper functioning of the prostate gland. In addition, testosterone plays a role in erection, allowing sperm to be deposited within the female reproductive tract.
HORMONAL CONTROL OF REPRODUCTION
The human male and female reproductive cycles are controlled by the interaction of hormones from the hypothalamus and anterior pituitary with hormones from reproductive tissues and organs. In both sexes, the hypothalamus monitors and causes the release of hormones from the anterior pituitary gland. When the reproductive hormone is required, the hypothalamus sends a gonadotropin-releasing hormone (GnRH) to the anterior pituitary. This causes the release of follicle stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary into the blood. Although these hormones are named after their functions in female reproduction, they are produced in both sexes and play important roles in controlling reproduction. Other hormones have specific functions in the male and female reproductive systems.
At the onset of puberty, the hypothalamus causes the release of FSH and LH into the male system for the first time. FSH enters the testes and stimulates the Sertoli cells located in the walls of the seminiferous tubules to begin promoting spermatogenesis ([link]). LH also enters the testes and stimulates the interstitial cells of Leydig, located in between the walls of the seminiferous tubules, to make and release testosterone into the testes and the blood.
A negative feedback system (Figure 14.13) occurs in the male with rising levels of testosterone acting on the hypothalamus and anterior pituitary to inhibit the release of GnRH, FSH, and LH. In addition, the Sertoli cells produce the hormone inhibin, which is released into the blood when the sperm count is too high. This inhibits the release of GnRH and FSH, which will cause spermatogenesis to slow down. If the sperm count reaches a low of 20 million/mL, the Sertoli cells cease the release of inhibin, and the sperm count increases.
Figure 14.13 Hormones control sperm production in a negative feedback system.
MY HUMAN BODY

If you’re a man and you use a laptop computer on your lap for long periods of time, you may be decreasing your fertility. The reason? A laptop computer generates considerable heat, and its proximity to the scrotum during typical use results in a significant rise in temperature inside the scrotum. Spermatogenesis is very sensitive to high temperatures, so it may be adversely affected by laptop computer use. If you want to avoid the potentially fertility-depressing effect of laptop computer use, you might want to consider using your laptop computer on a table or other surface rather than on your lap — at least when you log on for long computer sessions. Other activities that raise scrotal temperature and have the potential to reduce spermatogenesis including soaking in hot tubs, wearing tight clothing, and biking. Although the effects of short-term scrotal heating on fertility seem to be temporary, years of such heat exposure may cause irreversible effects on sperm production.
Review
Fill in the blanks:
are formed, and these must move to the ________________ where they will mature.
4. Describe semen and its components.
14.5 FEMALE REPRODUCTIVE ORGANS
The female reproductive system is made up of internal and external organs that function to produce haploid female gametes called ova (or oocytes), secrete female sex hormones (such as estrogen), and carry and give birth to a fetus. The internal female reproductive organs include the vagina, uterus, oviducts, and ovaries. The external organs — collectively called the vulva — include the clitoris and labia.
The vagina is an elastic, muscular canal leading from its opening in the vulva to the neck of the uterus, called the cervix. It is about 7.5 cm (about 3 in) long at the front, and about 9 cm (3.5 in) long at the back. The vagina accommodates the penis and is the site where sperm are usually ejaculated during sexual intercourse. In the context of pregnancy and natural (vaginal) childbirth, the vagina is referred to as the birth canal. In addition, it channels the flow of menstrual blood from the uterus.
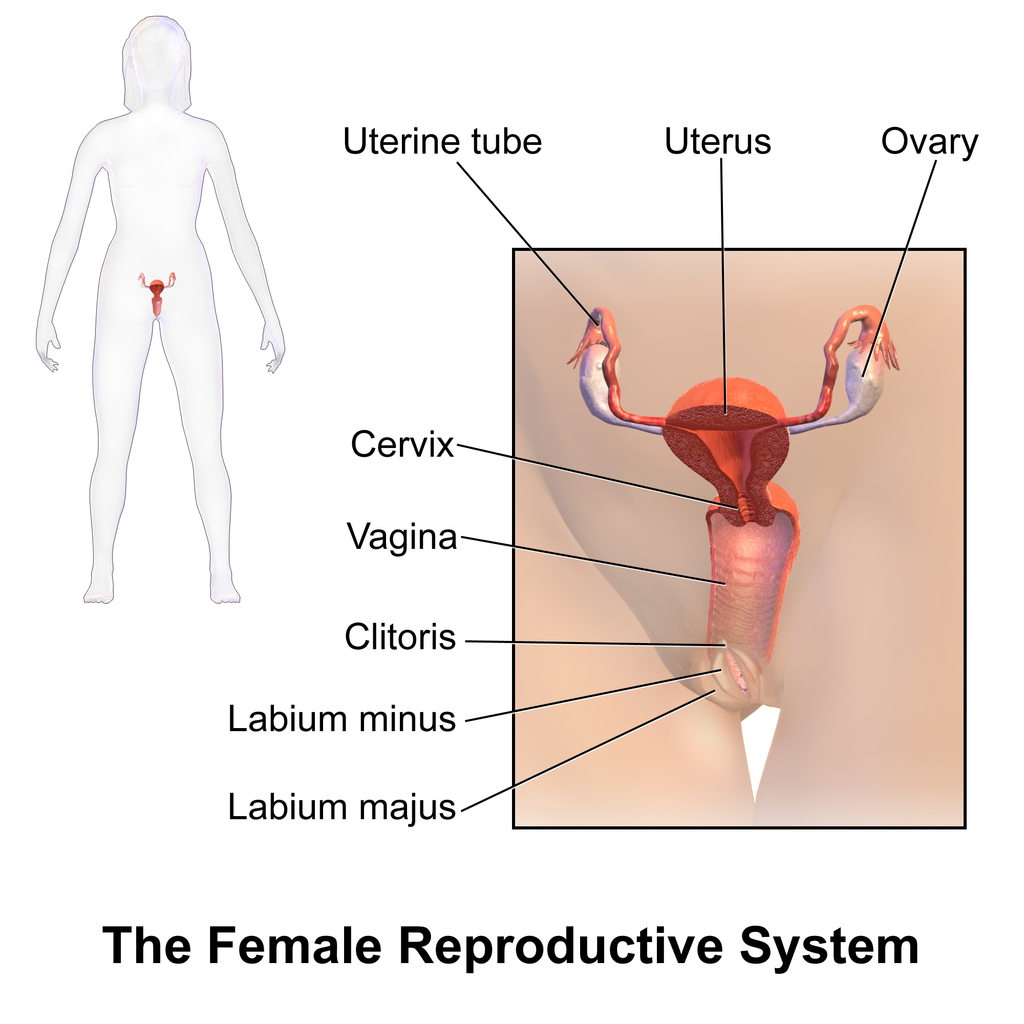
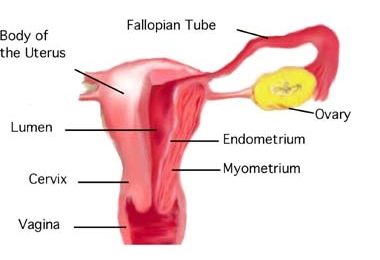
Figure 14.15 The main organs of the female reproductive system lie within the abdominal cavity.
STRUCTURE OF THE VAGINA
Muscles and ligaments support the vagina within the pelvic cavity. The vagina itself is made up of several layers of fibrous and muscular tissues and lined with mucous membranes. Folds in the mucosa provide the vagina with extra surface area so it can stretch in both length and width during intercourse or childbirth. The elasticity of the vagina and the extra mucosa allow it to stretch to many times its normal diameter in order to deliver a baby.
BACTERIA AND PH IN THE VAGINA
A healthy vagina is home to many symbiotic bacteria that help prevent pathogens (such as yeast) from colonizing the vagina. The pH in the vagina is normally between 3.8 and 4.5, and this acidity also helps keep pathogenic microorganisms from colonizing it. The vagina constantly sheds its epithelium, so it is considered self-cleaning. As a consequence, there is no need for douching to clean it. Physicians actually discourage the practice, as it may upset the normal bacterial and pH balance in the vagina, although washing the vulva with a mild soap is good practice.
UTERUS
The uterus (commonly called the womb) is a pear-shaped, muscular organ that is about 7.6 cm (about 3 in) long. It is located above the vagina and behind the bladder in the centre of the pelvis. The position of the uterus in the pelvis is stabilized by several ligaments and bands of supportive tissue. The uterus is where a fetus develops during gestation, and the organ provides mechanical protection and support for the developing offspring. Contractions of the muscular wall of the uterus are responsible for pushing the fetus out of the uterus during childbirth.
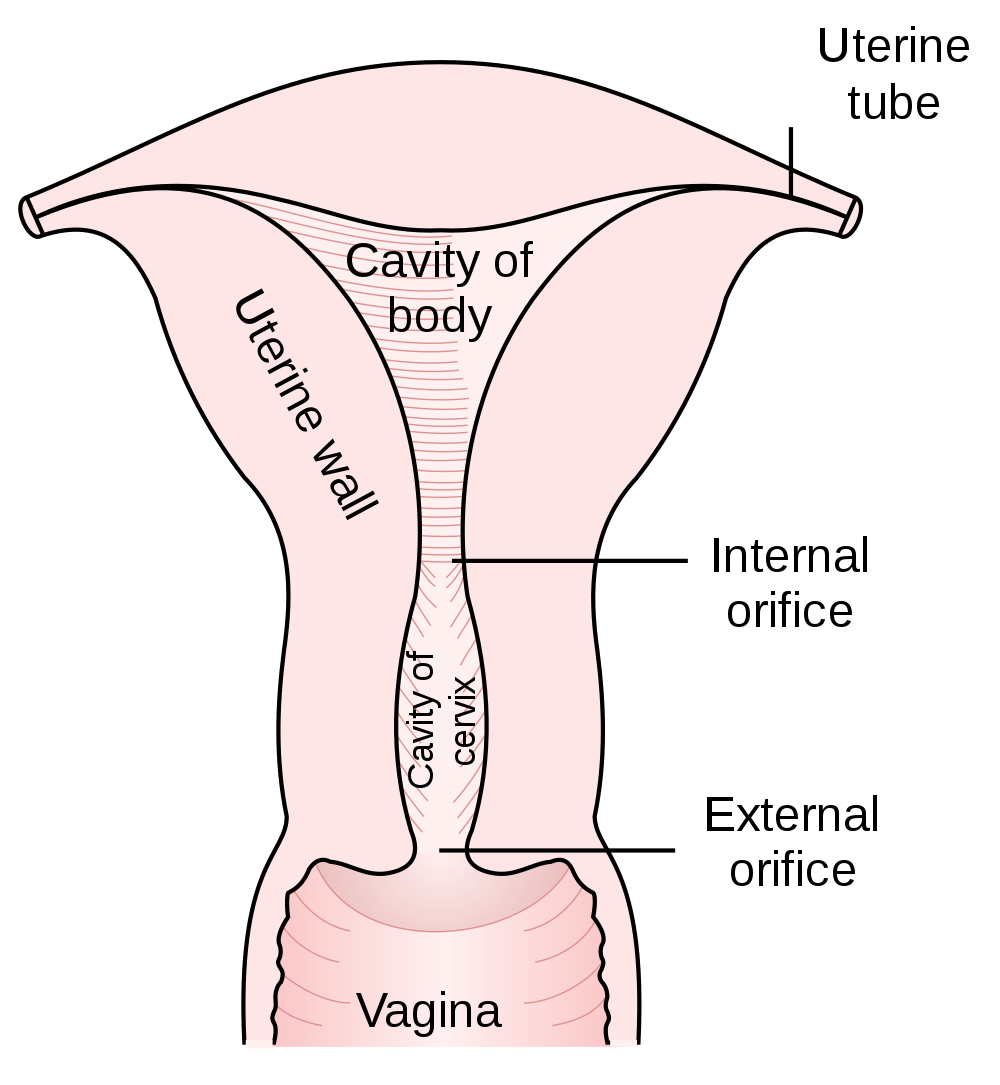
PARTS OF THE UTERUS
As shown in Figure 14.16, the lower end of the uterus forms the cervix, which is also called the neck of the uterus. The cervix is about 2.5 cm (almost 1 in) long and protrudes downward into the vagina. A small canal runs the length of the cervix, connecting the uterine cavity with the lumen of the vagina. This allows semen deposited in the vagina to enter the uterus, and a baby to pass from the uterus into the vagina during birth. Glands in the cervix secrete mucus that varies in water content and thickness, so it can function either as a barrier to keep microorganisms out of the uterus during pregnancy, or as a transport medium to help sperm enter the uterus around the time of ovulation. The rest of the uterus above the cervix is called the body of the uterus. The upper end of the uterus is connected with the two oviducts.
TISSUES OF THE UTERUS
As indicated in Figure 14.17, the uterus consists of three tissue layers, called the endometrium, myometrium, and perimetrium.
- The endometrium is the innermost tissue layer of the uterus. It consists of epithelial tissue, including mucous membranes. This layer thickens during each menstrual cycle and, unless an egg is fertilized, sloughs off during the following menstrual period. If an ovum is fertilized, the thickened endometrium is maintained by hormones and provides nourishment to the embryo. As gestation progresses, the endometrium develops into the maternal portion of the placenta.
- The placenta is a temporary organ that consists of a mass of maternal and fetal blood vessels through which the mother’s and fetus’s blood exchange substances.
- The myometrium is the middle layer of the uterus. It consists mostly of a thick layer of smooth muscle tissue. Powerful contractions of the smooth muscle allow the uterus to contract and expel an infant during childbirth.
- The perimetrium is the outermost layer of the uterus. It covers the outer surface of the uterus. This layer actually consists of two layers of epithelium that secrete fluid into the space between them. The fluid allows for small movements of the uterus within the pelvis, without causing it to rub against other organs.
OVIDUCTS
The oviducts (often referred to as Fallopian tubes) are two thin tubes that lie between the ovaries and the uterus. The oviducts are not attached to the ovaries, but their broad upper ends — called infundibula — lie very close to the ovaries. The infundibula also have fringe-like extensions called fimbriae that move in a waving motion to help guide eggs from the ovaries into the oviducts. The lower ends of the oviducts are attached to the upper part of the body of the uterus on either side of the body. They open into the uterus.
The oviducts are made up of multiple tissue layers. The innermost layer consists of mucosal epithelium. The epithelium is covered with cilia, which can move in a sweeping motion to help ova move through the tube from the ovary to the uterus. In between the ciliated cells of the epithelium are cells that secrete a fluid called tubular fluid. This fluid contains nutrients for sperm, ova, and zygotes. The secretions in tubular fluid also remove certain molecules from the plasma membrane of sperm so they are better able to penetrate an egg. Other layers of the oviducts consist of connective tissue and smooth muscle. Contractions of the smooth muscle allow peristalsis to help move eggs through the tubes.
Ovaries
Like the testes in males, the ovaries in females are gonads that produce gametes and secrete sex hormones. The gametes produced by the ovaries are called ova, or oocytes. The main sex hormone secreted by the ovaries is estrogen. The position of the paired ovaries relative to the other reproductive system organs is shown in Figure 14.18. Each ovary lies along one side of the uterus and is about 4 cm (a little more than 1.5 in) long. Fibrous ligaments attach one end of each ovary to its nearby oviduct and the other and to its side of the uterus. These ligaments keep the ovaries in place within the pelvis.
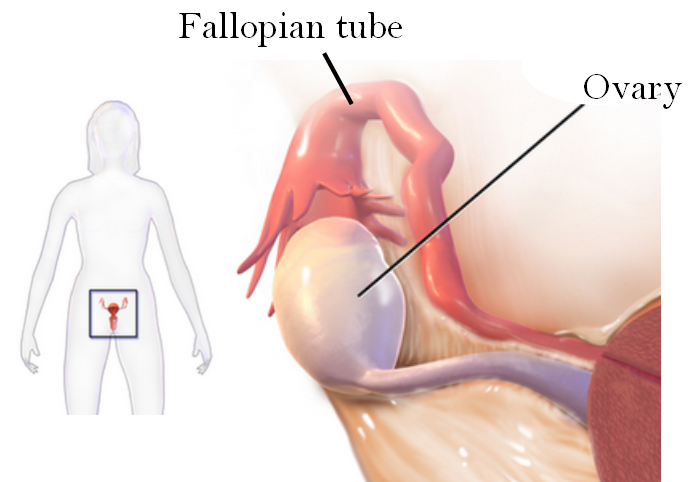
Figure 14.18 The placement of the two ovaries within the pelvis allows eggs from each ovary to enter a Fallopian tube and travel to the uterus.
OVARIAN FOLLICLES
The ovary consists of two main layers, called the ovarian medulla (the inner layer) and the ovarian cortex (the outer layer). The ovary also contains blood and lymphatic vessels. The ovarian cortex consists primarily of the functional units of the ovaries, which are called ovarian follicles. The follicles are nests of epithelial cells, within each of which is an ovum. The photomicrograph in Figure 14.18 shows an ovarian follicle and the developing ovum inside it. If an ovum and follicle complete maturation, the follicle ruptures and the ovum is released from the ovary. This event is called ovulation.
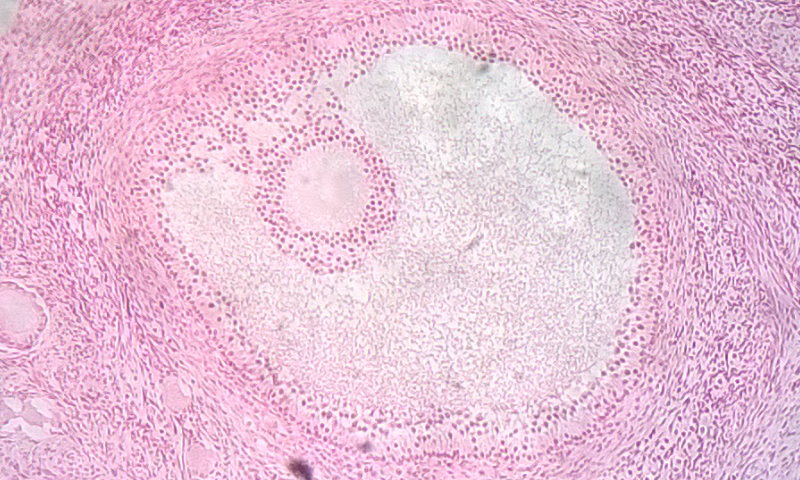
Figure 14.19 An ovum within its nest of follicular cells inside an ovary.
OVA IN THE OVARIES
Whereas the male testes produce sperm continuously after puberty, the female ovary already contains all the ova it will ever produce by the time a female is born. At birth, a baby girl’s ovaries contain at least a million eggs, each of which is contained within a follicle. Only about 500 of these eggs will eventually mature and be ovulated. This process starts at puberty and typically continues at monthly intervals until menopause occurs around age 52. The remaining eggs never mature, and their number declines as the woman ages. By menopause, a woman’s reserve of eggs is nearly depleted, and ovulation no longer occurs.
VULVA
The vulva is a general term for all of the external female reproductive organs. The vulva includes the clitoris, labia, and external openings for the urethra and vagina.
LABIA
The labia (singular, labium) refer to the “lips” of the vulva, which are folds of tissue that contain and protect the other, more delicate structures of the vulva (as shown in Figure 14.20). There are two pairs of labia: the outer and larger labia majora, and the inner and smaller labia minora. The labia minora contain numerous sebaceous glands. These glands release secretions that help lubricate the labia and vulvar area.
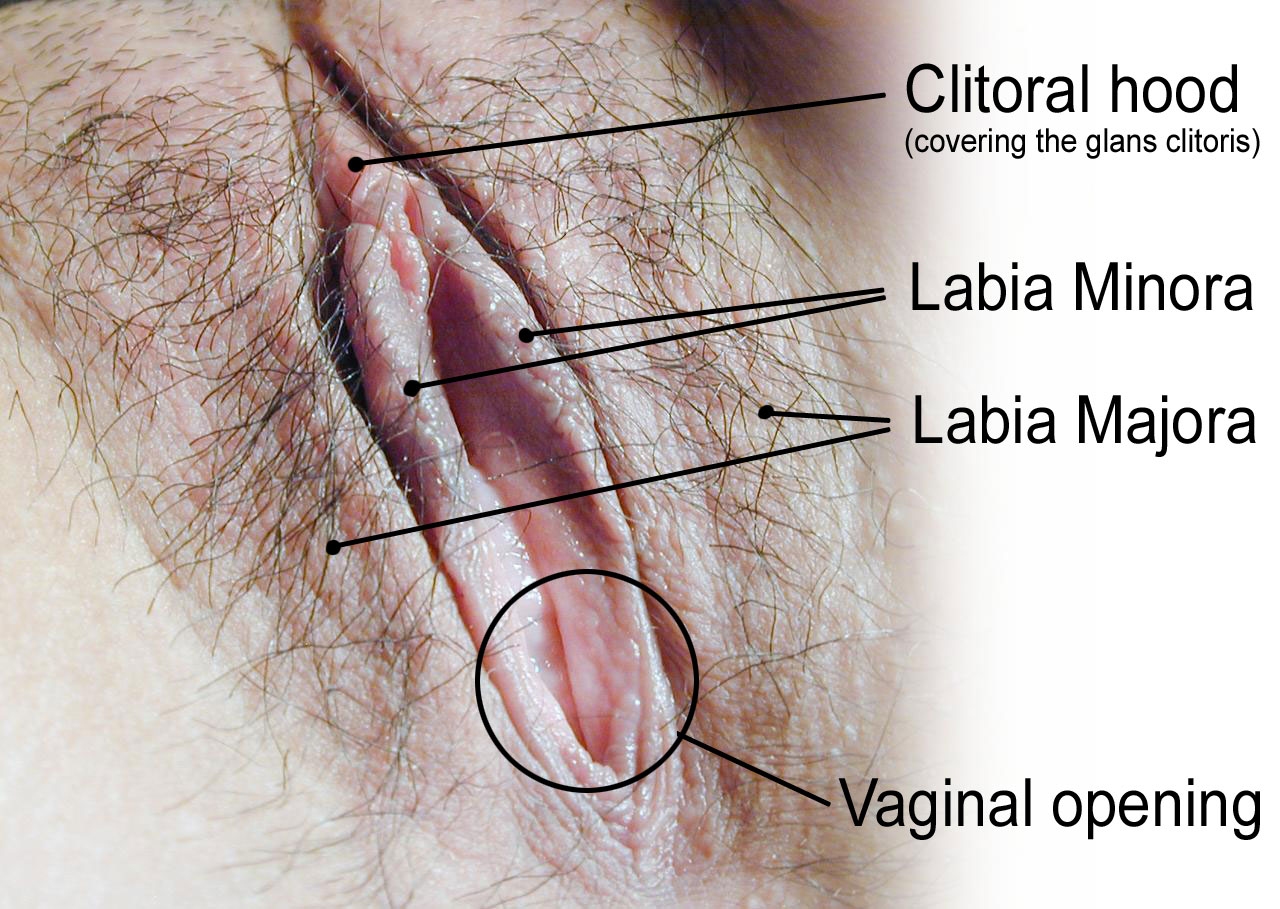
Figure 14.20 The vulva includes the external features of the female reproductive system including the labia, clitoris and clitoral hood, and the openings from the urethra and to the vagina.
CLITORIS
The clitoris is located at the front of the vulva where the labia minora meet. The visible portion of the clitoris is called the glans clitoris. It is roughly the size and shape of a pea. It is highly sensitive, because it contains many nerve endings. The clitoris is the homologue to the male penis, and they both contain spongy tissue. Stimulation of the glans clitoris during sexual activity generally results in sexual arousal in females and may lead to orgasm. The glans clitoris is the only part of the overall clitoris visible externally, but this spongy tissue extends down either side of the openings to the urethra and vagina.
OTHER VULVAR STRUCTURES
The area between the two labia minora is called the vestibule of the vulva. Both the urethra and vagina have openings to the outside of the body in the vestibule. The urethral opening is located just in front of, and is much smaller than, the vaginal opening. Both openings are protected by the labia. Two glands — called Bartholin’s glands — open on either side of the vaginal opening. These glands secrete mucus and a vaginal and vulvar lubricant.
BREASTS
The breasts are not directly involved in reproduction, but because they contain mammary glands, they can provide nourishment to an infant after birth. The breasts overlay major muscles in the chest from which they project outward in a conical shape. The two main types of tissues in the breast are adipose (fat) tissue and glandular tissue that produces milk. As shown in Figure 14.21, each mature breast contains many lobules, where milk is produced and stored during pregnancy. During breastfeeding (or lactation), the milk drains into ducts and sacs, which in turn converge at the nipple. Milk exits the breast through the nipple in response to the suckling action of an infant and is regulated by a positive feedback loop. The nipple is surrounded by a more darkly pigmented area called the areola. The areola contains glands that secrete an oily fluid, which lubricates and protects the nipple during breastfeeding.
Human Physiology – Functional Anatomy of the Female Reproductive System.
Review
Fill in the blanks
14.6 FUNCTIONS OF THE FEMALE REPRODUCTIVE SYSTEM
At birth, a female’s ovaries contain all the ova she will ever produce, which may include a million or more ova. The ova don’t start to mature, however, until she enters puberty and attains sexual maturity. After that, one ovum typically matures each month, and is released from an ovary. This continues until a woman reaches menopause (cessation of monthly periods), typically by age 52. By then, viable eggs may be almost depleted, and hormone levels can no longer support the monthly cycle. During the reproductive years, which of the two ovaries releases an egg in a given month seems to be a matter of chance. Occasionally, both ovaries will release an egg at the same time. If both eggs are fertilized, the offspring are fraternal twins (dizygotic, or “two-zygote,” twins), and they are no more alike genetically than non-twin siblings.
OOGENESIS
The process of producing ova in the ovaries of a female fetus is called oogenesis. Ova are haploid gametes, and their production occurs in several steps that involve different types of cells. Oogenesis is completed long before birth. It occurs when diploid germ cells called oogonia (singular, oogonium) undergo mitosis. Each such cell division produces two diploid daughter cells. One is called the primary oocyte, and the other is retained to help maintain a reserve of oogonia. The primary oocyte, in turn, starts to go through the first cell division of meiosis (meiosis I). However, it does not complete meiosis I until much later. Instead, it remains in a resting state, nestled within a tiny, immature follicle in the ovary until the female goes through puberty.
MATURATION OF A FOLLICLE
Beginning in puberty, about once a month, one of the follicles in an ovary undergoes maturation, and an egg is released. As the follicle matures, it goes through changes in the numbers and types of its cells, as shown in Figure 14.22. The primary oocyte within the follicle also resumes meiosis. It completes meiosis I, which began long before birth, to form a secondary oocyte and a smaller cell, called the first polar body. Both the secondary oocyte and the first polar body are haploid cells. The secondary oocyte has most of the cytoplasm from the primary oocyte and is much larger than the first polar body, which soon disintegrates and disappears. The secondary oocyte begins meiosis II, but only completes it if the egg is fertilized.
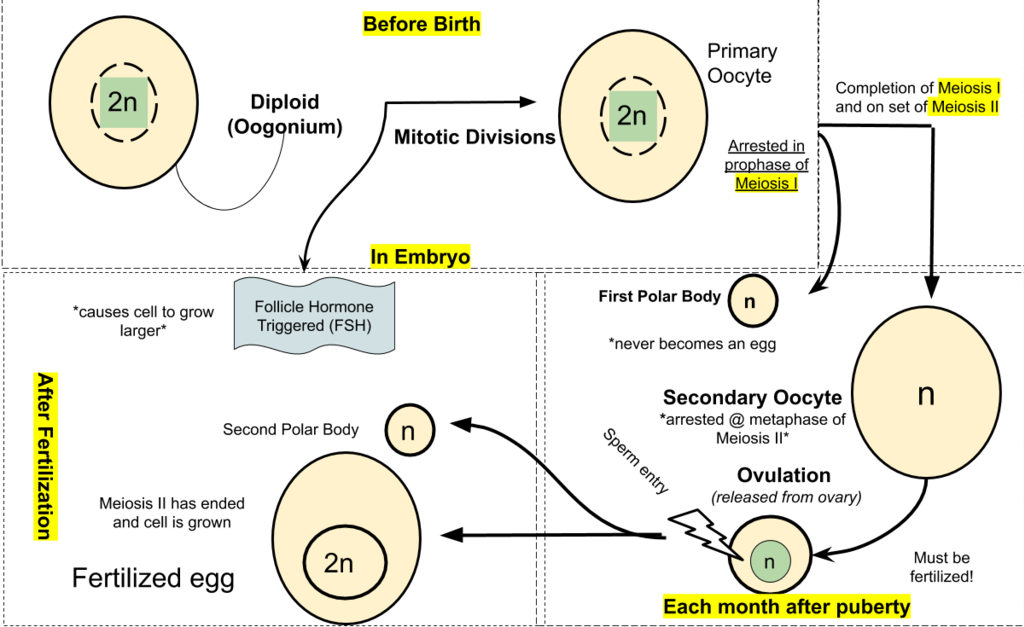
RELEASE OF AN EGG
It typically takes 12 to 14 days for a follicle to mature in an ovary, and for the secondary oocyte to form. Then, the follicle bursts open and the ovary ruptures, releasing the secondary oocyte from the ovary. This event is called ovulation. The now-empty follicle starts to change into a structure called a corpus luteum. The expelled secondary oocyte is usually swept into the nearby oviduct by its waving, fringe-like fimbriae.
UTERINE CHANGES
While the follicle is maturing in the ovary, the uterus is also undergoing changes to prepare it for an embryo if fertilization occurs. For example, the endometrium gets thicker and becomes more vascular. Around the time of ovulation, the cervix undergoes changes that help sperm reach the ovum to fertilize it. The cervical canal widens, and cervical mucus becomes thinner and more alkaline. These changes help promote the passage of sperm from the vagina into the uterus and make the environment more hospitable to sperm.
FERTILIZATION — OR NOT
Fertilization of an ovum by a sperm normally occurs in an oviduct, most often in the part of the tube that passes above the ovary (see Figure 14.23). In order for fertilization to occur, sperm must “swim” from the vagina where they are deposited, through the cervical canal to the uterus, and then through the body of the uterus to one of the oviducts. Once sperm enter a oviduct, tubular fluids help carry them through the tube toward the secondary oocyte at the other end. The secondary oocyte also functions to promote fertilization. It releases molecules that guide the sperm and allow the surface of the ovum to attach to the surface of the sperm. The ovum can then absorb the sperm, allowing fertilization to occur.
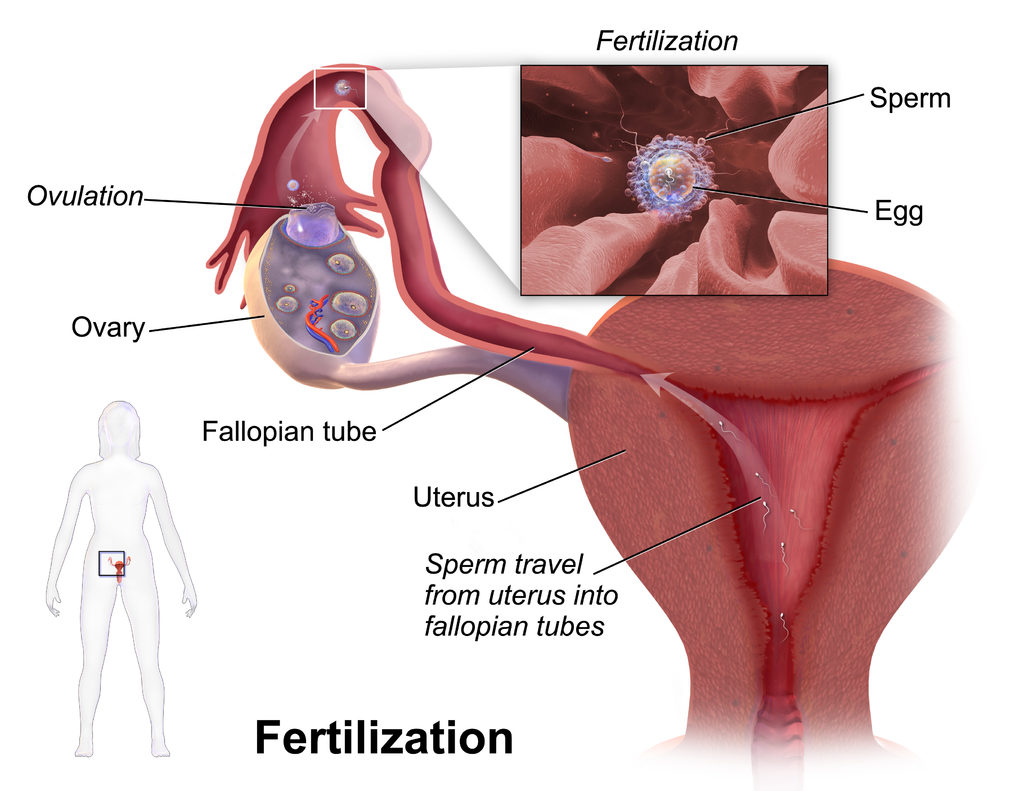
IF FERTILIZATION OCCURS
If the secondary oocyte is fertilized by a sperm as it passes through the oviduct, the secondary oocyte quickly completes meiosis II, forming a diploid zygote and another polar body. This second polar body, like the first, normally breaks down and disappears. The zygote then continues the journey through the oviduct to the uterus, during which it undergoes several mitotic cell divisions. By the time it reaches the uterus up to five days after fertilization, it consists of a ball of cells called a blastocyst. Within another day or two, the blastocyst implants itself in the endometrium lining the uterus, and gestation begins.
IF FERTILIZATION DOES NOT OCCUR
What happens if the secondary oocyte is not fertilized by a sperm as it passes through the oviduct? It continues on its way to the uterus without ever completing meiosis II. It is likely to disintegrate within a few days while still in the oviduct. Any remaining material will be shed from the woman’s body during the next menstrual period.
Fertilization Video
PREGNANCY AND CHILDBIRTH
Pregnancy is the carrying of one or more offspring from fertilization until birth. This is one of the major functions of the female reproductive system. It involves virtually every other body system including the cardiovascular, urinary, and respiratory systems, to name just three. The maternal organism plays a critical role in the development of the offspring. She must provide all the nutrients and other substances needed for normal growth and development of the offspring, and she must also remove the wastes excreted by the offspring. Most nutrients are needed in greater amounts by a pregnant woman to meet fetal needs, but some are especially important, including folic acid, calcium, iron, and omega-3 fatty acids. A healthy diet), along with prenatal vitamin supplements, is recommended for the best pregnancy outcome. A pregnant woman should also avoid ingesting substances (such as alcohol) that can damage the developing offspring, especially early in the pregnancy when all of the major organs and organ systems are forming.
FEMALE SEX HORMONES
Female reproduction could not occur without sex hormones released by the ovaries. These hormones include estrogen and progesterone.
ESTROGEN
Before birth, estrogen is released by the gonads in female fetuses and leads to the development of female reproductive organs. At puberty, estrogen levels rise and are responsible for sexual maturation, and for the development of female secondary sex characteristics (such as breasts). Estrogen is also needed to help regulate the menstrual cycle and ovulation throughout a woman’s reproductive years. Estrogen is produced primarily by follicular cells in the ovaries. During pregnancy, estrogen is also produced by the placenta.
PROGESTERONE
Progesterone stands for “pro-gestational hormone.” It is synthesized and secreted primarily by the corpus luteum in the ovary. Progesterone plays many physiological roles but is best known for its role during pregnancy. In fact, it is sometimes called the “hormone of pregnancy.” Among other functions, progesterone prepares the uterus for pregnancy each month by building up the uterine lining. If a pregnancy occurs, progesterone helps maintain the pregnancy in a number of ways, such as decreasing the maternal immune response to the genetically different embryo and decreasing the ability of uterine muscle tissue to contract. Progesterone also prepares the mammary glands for lactation during pregnancy, and withdrawal of progesterone after birth is one of the triggers of milk production.
Review
1. Identify the functions of the female sex hormones estrogen and progesterone.
3. Fill in the blanks:
_______________ is the development of ova through the process of meiosis. It takes place in the __________________
During this time, the uterus has been preparing to house the zygote by building up the lining called the ___________________.
14.7 MENSTRUAL CYCLE
WHAT IS THE MENSTRUAL CYCLE?
The menstrual cycle refers to natural changes that occur in the female reproductive system each month during the reproductive years. The cycle is necessary for the production of ova and the preparation of the uterus for pregnancy. It involves changes in both the ovaries and the uterus, and is controlled by pituitary and ovarian hormones. Day 1 of the cycle is the first day of the menstrual period, when bleeding from the uterus begins as the built-up endometrium lining the uterus is shed. The endometrium builds up again during the remainder of the cycle, only to be shed again during the beginning of the next cycle if pregnancy does not occur. In the ovaries, the menstrual cycle includes the development of a follicle, ovulation of a secondary oocyte, and then degeneration of the follicle if pregnancy does not occur. Both uterine and ovarian changes during the menstrual cycle are generally divided into three phases, although the phases are not the same in the two organs.
MENARCHE AND MENOPAUSE
The female reproductive years are delineated by the start and stop of the menstrual cycle. The first menstrual period usually occurs around 12 or 13 years of age, an event that is known as menarche. There is considerable variation among individuals in the age at menarche. It may occasionally occur as early as eight years of age or as late as 16 years of age and still be considered normal. The average age is generally later in the developing world, and earlier in the developed world. This variation is thought to be largely attributable to nutritional differences.
The cessation of menstrual cycles at the end of a woman’s reproductive years is termed menopause. The average age of menopause is 52 years, but it may occur normally at any age between about 45 and 55 years of age. The age of menopause varies due to a variety of biological and environmental factors. It may occur earlier as a result of certain illnesses or medical treatments.
VARIATION IN THE MENSTRUAL CYCLE
The length of the menstrual cycle — as well as its phases — may vary considerably, not only among different women, but also from month to month for a given woman. The average length of time between the first day of one menstrual period and the first day of the next menstrual period is 28 days, but it may range from 21 days to 45 days. Cycles are considered regular when a woman’s longest and shortest cycles differ by less than eight days. The menstrual period itself is usually about five days long, but it may vary in length from about two days to seven days.
OVARIAN CYCLE
The events of the menstrual cycle that take place in the ovaries make up the ovarian cycle. It consists of changes that occur in the follicles of one of the ovaries. The ovarian cycle is divided into the following three phases: follicular phase, ovulation, and luteal phase. These phases are illustrated in Figure 14.23.
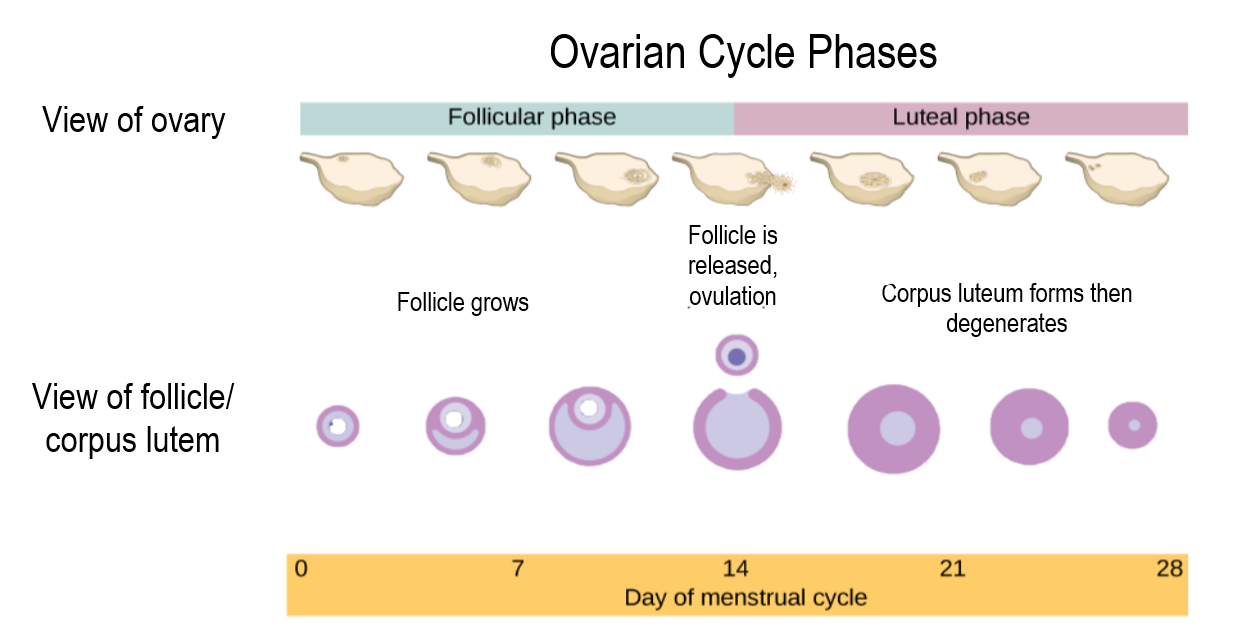
FOLLICULAR PHASE
The follicular phase is the first phase of the ovarian cycle. It generally lasts about 12 to 14 days for a 28-day menstrual cycle. During this phase, several ovarian follicles are stimulated to begin maturing, but usually only one — called the Graafian follicle — matures completely so it is ready to release an egg. The other maturing follicles stop growing and disintegrate. Follicular development occurs because of a rise in the blood level of follicle stimulating hormone (FSH), which is secreted by the pituitary gland. The maturing follicle releases estrogen, the level of which rises throughout the follicular phase. You can see these and other changes in hormone levels that occur during the menstrual cycle in the following chart.
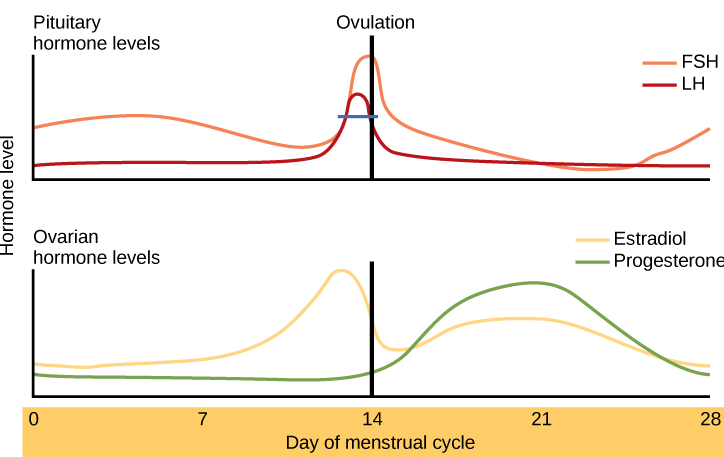
OVULATION
Ovulation is the second phase of the ovarian cycle. It usually occurs around day 14 of a 28-day menstrual cycle. During this phase, the Graafian follicle ruptures and releases its ovum. Ovulation is stimulated by a sudden rise in the blood level of luteinizing hormone (LH) from the pituitary gland. This is called the LH surge. You can see the LH surge in the top hormone graph in Figure 18.8.3. The LH surge generally starts around day 12 of the cycle and lasts for a day or two. The surge in LH is triggered by a continued rise in estrogen from the maturing follicle in the ovary. During the follicular phase, the rising estrogen level actually suppresses LH secretion by the pituitary gland. However, by the time the follicular phase is nearing its end, the level of estrogen reaches a threshold level above which this effect is reversed, and estrogen stimulates the release of a large amount of LH. The surge in LH matures the ovum and weakens the wall of the follicle, causing the fully developed follicle to release its secondary oocyte.
LUTEAL PHASE
The luteal phase is the third and final phase of the ovarian cycle. It typically lasts about 14 days in a 28-day menstrual cycle. At the beginning of the luteal phase, FSH and LH cause the Graafian follicle that ovulated the egg to transform into a structure called a corpus luteum. The corpus luteum secretes progesterone, which in turn suppresses FSH and LH production by the pituitary gland and stimulates the continued buildup of the endometrium in the uterus. How this phase ends depends on whether or not the ovum has been fertilized.
- If fertilization has not occurred, the falling levels of FSH and LH during the luteal phase cause the corpus luteum to atrophy, so its production of progesterone declines. Without a high level of progesterone to maintain it, the endometrium starts to break down. By the end of the luteal phase, the endometrium can no longer be maintained, and the next menstrual cycle begins with the shedding of the endometrium (menses).
- If fertilization has occurred so a zygote forms and then divides to become a blastocyst, the outer layer of the blastocyst produces a hormone called human chorionic gonadotropin (HCG). This hormone is very similar to LH and preserves the corpus luteum. The corpus luteum can then continue to secrete progesterone to maintain the new pregnancy.
UTERINE CYCLE
The events of the menstrual cycle that take place in the uterus make up the uterine cycle. This cycle consists of changes that occur mainly in the endometrium, which is the layer of tissue that lines the uterus. The uterine cycle is divided into the following three phases: menstruation, proliferative phase, and secretory phase. These phases are illustrated in Figure 14.25.
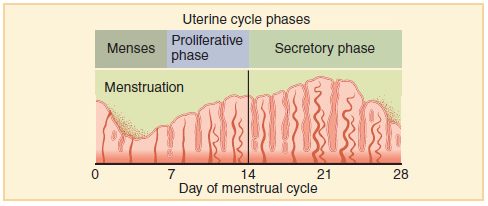
MENSTRUATION
Menstruation (also called menstrual period or menses) is the first phase of the uterine cycle. It occurs if fertilization has not taken place during the preceding menstrual cycle. During menstruation, the endometrium of the uterus, which has built up during the preceding cycle, degenerates and is shed from the uterus, flowing through an opening in the cervix, and out through the external opening of the vagina. The average loss of blood during menstruation is about 35 mL (about 1 oz or 2 tablespoons). The flow of blood is often accompanied by uterine cramps, which may be severe in some women.
PROLIFERATIVE PHASE
The proliferative phase is the second phase of the uterine cycle. During this phase, estrogen secreted by cells of the maturing ovarian follicle causes the lining of the uterus to grow or proliferate. Estrogen also stimulates the cervix of the uterus to secrete larger amounts of thinner mucus that can help sperm swim through the cervix and into the uterus, making fertilization more likely.
SECRETORY PHASE
The secretory phase is the third and final phase of the uterine cycle. During this phase, progesterone produced by the corpus luteum in the ovary stimulates further changes in the endometrium so it is more receptive to implantation of a blastocyst. For example, progesterone increases blood flow to the uterus and promotes uterine secretions. It also decreases the contractility of smooth muscle tissue in the uterine wall.
BRINGING IT ALL TOGETHER
It is important to note that the pituitary gland, the ovaries and the uterus are all responsible for parts of the ovarian and uterine cycles. The pituitary hormones, LH and FSH affect the ovarian cycle and its hormones. The ovarian hormones, estrogen and progesterone affect the uterine cycle and also feedback on the pituitary gland. Look at Figure 14.26 and look at what is happening on different days of the cycle in each of the sets of hormones, the ovarian cycle and the uterine cycle.
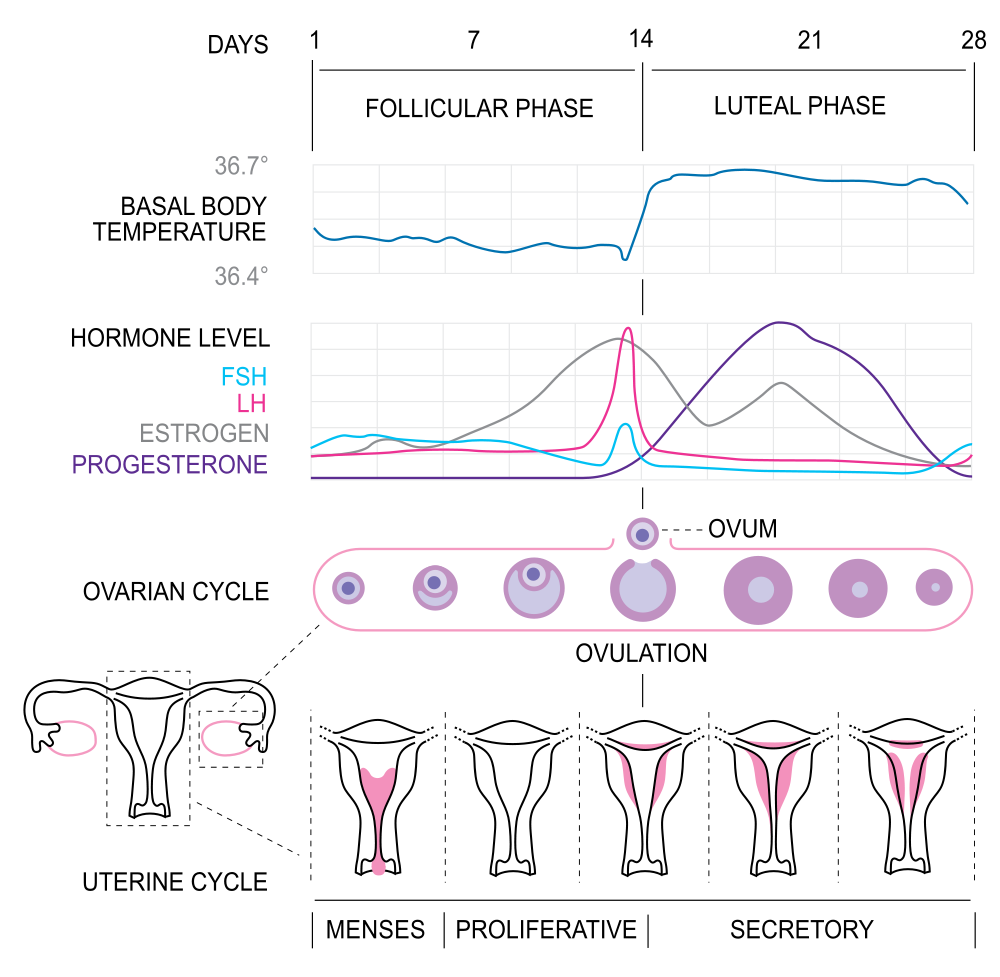
HORMONAL CONTROL OF REPRODUCTION
The control of reproduction in females is more complex and is regulated by both positive and negative feedback mechanisms. As with the male, gonadotropin releasing hormone (GnRH) is released by the hypothalamus and the anterior pituitary releases the hormones FSH and LH. In addition, estrogens and progesterone are released from the developing follicles. During most of the menstrual cycle, estrogen and progesterone levels slowly increase and inhibit the release of GnRH, FSH and LH as you would expect in a negative feedback mechanism.
The first half (Follicular Phase) of the menstrual cycle is regulated by a positive feedback mechanism. The high and rapidly increasing level of estrogen just prior to the middle (approximately day 14) of the cycle stimulates a spike in LH and causes ovulation to occur. The ruptured follicle forms into the corpus luteum and progesterone levels increase. The corpus luteum produces estrogen and progesterone. The progesterone facilitates the regrowth of the uterine lining and inhibits the release of further FSH and LH. In the second half (Luteal Phase) of the menstrual cycle, the cycle is under control of the negative feedback mechanism. The inhibition of FSH and LH prevents any further eggs and follicles from developing, while the progesterone is elevated. this prevents a second ovulation from occurring until the end of the cycle and the hormones estrogen and progesterone levels decrease to low levels again.
If no fertilized egg is implanted into the uterus, the corpus luteum degenerates and the levels of estrogen and progesterone decrease. The endometrium begins to degenerate as the progesterone levels drop, initiating the next menstrual cycle. The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, releasing FSH and LH and starting the cycles again.
Figure 14.27 The ovarian and menstrual cycles of female reproduction are regulated by hormones produced by the hypothalamus, pituitary, and ovaries.
Menopause
As people with ovarian reproductive systems approach their mid-40s to mid-50s, their ovaries begin to lose their sensitivity to FSH and LH. Menstrual periods become less frequent and finally cease; this is menopause. There are still eggs and potential follicles on the ovaries, but without the stimulation of FSH and LH, they will not produce a viable egg to be released. One outcome of this is the inability to have children.
The side effects of menopause include hot flashes, heavy sweating (especially at night), headaches, some hair loss, muscle pain, vaginal dryness, insomnia, depression, weight gain, and mood swings. Estrogen is involved in calcium metabolism and, without it, blood levels of calcium decrease. To replenish the blood, calcium is lost from bone which may decrease the bone density and lead to osteoporosis. Supplementation of estrogen in the form of hormone replacement therapy (HRT) can prevent bone loss, but the therapy can have negative side effects. While HRT is thought to give some protection from colon cancer, osteoporosis, heart disease, macular degeneration, and possibly depression, its negative side effects include increased risk of stroke or heart attack, blood clots, breast cancer, ovarian cancer, endometrial cancer, gall bladder disease, and possibly dementia.
Review
- What is the menstrual cycle? Why is the menstrual cycle necessary in order for pregnancy to occur?
- What organs are involved in the menstrual cycle?
- Identify the two major events that mark the beginning and end of the reproductive period in females. When do these events typically occur?
- Discuss the average length of the menstrual cycle and menstruation, as well as variations that are considered normal.
- If the LH surge did not occur in a menstrual cycle, what do you think would happen? Explain your answer.
- Give one reason why FSH and LH levels drop in the luteal phase of the menstrual cycle.
- How is the female reproductive system regulated by a positive feedback system?
- What is menopause?
14.8 INFERTILITY
Infertility is the inability of a sexually mature adult to reproduce by natural means. For scientific and medical purposes, infertility is generally defined as the failure to achieve a successful pregnancy after at least one year of regular, unprotected sexual intercourse. Infertility may be primary or secondary. Primary infertility applies to cases in which an individual has never achieved a successful pregnancy. Secondary infertility applies to cases in which an individual has had at least one successful pregnancy but fails to achieve another after trying for at least a year. Infertility is a common problem.
CAUSES OF INFERTILITY
Pregnancy is the result of a multi-step process. In order for a normal pregnancy to occur, a woman must release an ovum from one of her ovaries, the ovum must go through an oviduct, a man’s sperm must fertilize the ovum as it passes through the oviduct, and then the resulting zygote must implant in the uterus. If there is a problem with any of these steps, infertility can result.
A couple’s infertility may be due to a problem with either the male or the female partner. About 40% of infertility cases are due to female infertility, and about 30% are due to male infertility. The remaining 30% of cases are due to a combination of male and female problems or unknown causes.
CAUSES OF MALE INFERTILITY
Male infertility occurs when there are no, or too few, sperm, or when the sperm are not healthy and motile and cannot travel through the female reproductive tract to fertilize an egg. A common cause of inadequate numbers or motility of sperm is varicocele, which is enlargement of blood vessels in the scrotum. This may raise the temperature of the testes and adversely affect sperm production. In other cases, there is no problem with the sperm, but there is a blockage in the male reproductive tract that prevents the sperm from being ejaculated.
Factors that increase a man’s risk of infertility include heavy alcohol use, drug abuse, cigarette smoking, exposure to environmental toxins (such as pesticides or lead), certain medications, serious diseases (such as kidney disease), and radiation or chemotherapy for cancer. Another risk factor is advancing age. Male fertility normally peaks in the mid-twenties and gradually declines after about age 40, although it may never actually drop to zero.
CAUSES OF FEMALE INFERTILITY
Female infertility generally occurs due to one of two problems: failure to produce viable ova by the ovaries, or structural problems in the oviducts or uterus. The most common cause of female infertility is a problem with ovulation. Without ovulation, there are no ova to be fertilized. Anovulatory cycles (menstrual cycles in which ovulation does not occur) may be associated with no or irregular menstrual periods, but even regular menstrual periods may be anovulatory for a variety of reasons. The most common cause of anovulatory cycles is polycystic ovary syndrome (PCOS), which causes hormone imbalances that can interfere with normal ovulation. Another relatively common cause of anovulation is primary ovarian insufficiency. In this condition, the ovaries stop working normally and producing viable eggs at a relatively early age, generally before the age of 40.
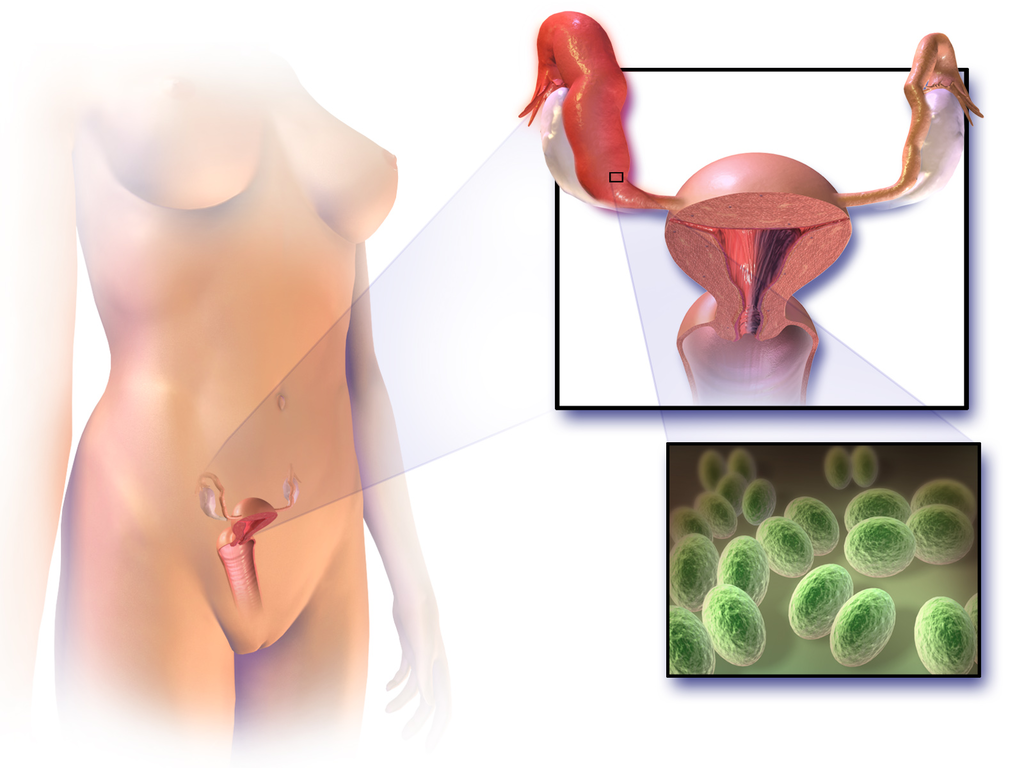
Structural problems with the oviducts or uterus are less common causes of female infertility. The oviducts may be blocked as a result of endometriosis. Another possible cause is pelvic inflammatory disease, which occurs when sexually transmitted infections spread to the oviducts or other female reproductive organs (see Figure 14.28). The infection may lead to scarring and blockage of the oviducts. If an ovum is produced and the oviducts are functioning — and a woman has a condition such as uterine fibroids — implantation in the uterus may not be possible. Uterine fibroids are non-cancerous clumps of tissue and muscle that form on the walls of the uterus.
Factors that increase a woman’s risk of infertility include tobacco smoking, excessive use of alcohol, stress, poor diet, strenuous athletic training, and being overweight or underweight. Advanced age is even more problematic for females than males. Female fertility normally peaks in the mid-twenties, and continuously declines after age 30 and until menopause around the age of 52, after which the ovary no longer releases eggs. About 1/3 of couples in which the woman is over age 35 have fertility problems. In older women, more cycles are likely to be anovulatory, and the eggs may not be as healthy.
DIAGNOSING CAUSES OF INFERTILITY
Diagnosing the cause(s) of a couple’s infertility often requires testing both the man and the woman for potential problems. In men, the semen is likely to be examined for the number, shape, and motility of sperm. If problems are found with sperm, further studies are likely to be done, such as medical imaging to look for structural problems with the testes or ducts.
In women, the first step is most often determining whether ovulation is occurring. This can be done at home by carefully monitoring body temperature (it rises slightly around the time of ovulation) or using a home ovulation test kit, which is available over the counter at most drugstores. Whether or not ovulation is occurring can also be detected with blood tests or ultrasound imaging of the ovaries. If ovulation is occurring normally, then the next step may be an X-ray of the oviducts and uterus to see if there are any blockages or other structural problems. Another approach to examining the female reproductive tract for potential problems is laparoscopy. In this surgical procedure, a tiny camera is inserted into the woman’s abdomen through a small incision. This allows the doctor to directly inspect the reproductive organs.
TREATING INFERTILITY
Infertility often can be treated successfully. The type of treatment depends on the cause of infertility.
TREATING MALE INFERTILITY
Medical problems that interfere with sperm production may be treated with medications or other interventions that may lead to the resumption of normal sperm production. If, for example, an infection is interfering with sperm production, then antibiotics that clear up the infection may resolve the problem. If there is a blockage in the male reproductive tract that prevents the ejaculation of sperm, surgery may be able to remove the blockage. Alternatively, the man’s sperm may be removed from his body and then used for artificial insemination of his partner. In this procedure, the sperm are injected into the woman’s reproductive tract.
TREATING FEMALE INFERTILITY
In females, it may be possible to correct blocked Fallopian tubes or uterine fibroids with surgery. Ovulation problems, on the other hand, are usually treated with hormones that act either on the pituitary gland or on the ovaries. Hormonal treatments that stimulate ovulation often result in more than one egg being ovulated at a time, thus increasing the chances of a woman having twins, triplets, or even higher multiple births. Multiple fetuses are at greater risk of being born too early or having health and developmental problems. The mother is also at greater risk of complications arising during pregnancy. Therefore, the possibility of multiple fetuses should be weighed in making a decision about this type of infertility treatment.
ASSISTED REPRODUCTIVE TECHNOLOGY
Some cases of infertility are treated with assisted reproductive technology (ART). This is a collection of medical procedures in which ova are removed from the woman’s body and sperm are taken from the man’s body to be manipulated in ways that increase the chances of fertilization occurring. The eggs and sperm may be injected into one of the woman’s oviducts for fertilization to take place in vivo (in the body). More commonly, however, the eggs and sperm are mixed together outside the body, so fertilization takes place in vitro (in a test tube or dish in a lab). The latter approach is illustrated in Figure 14.29. With in vitro fertilization, the fertilized eggs may be allowed to develop into embryos before being placed in the woman’s uterus.
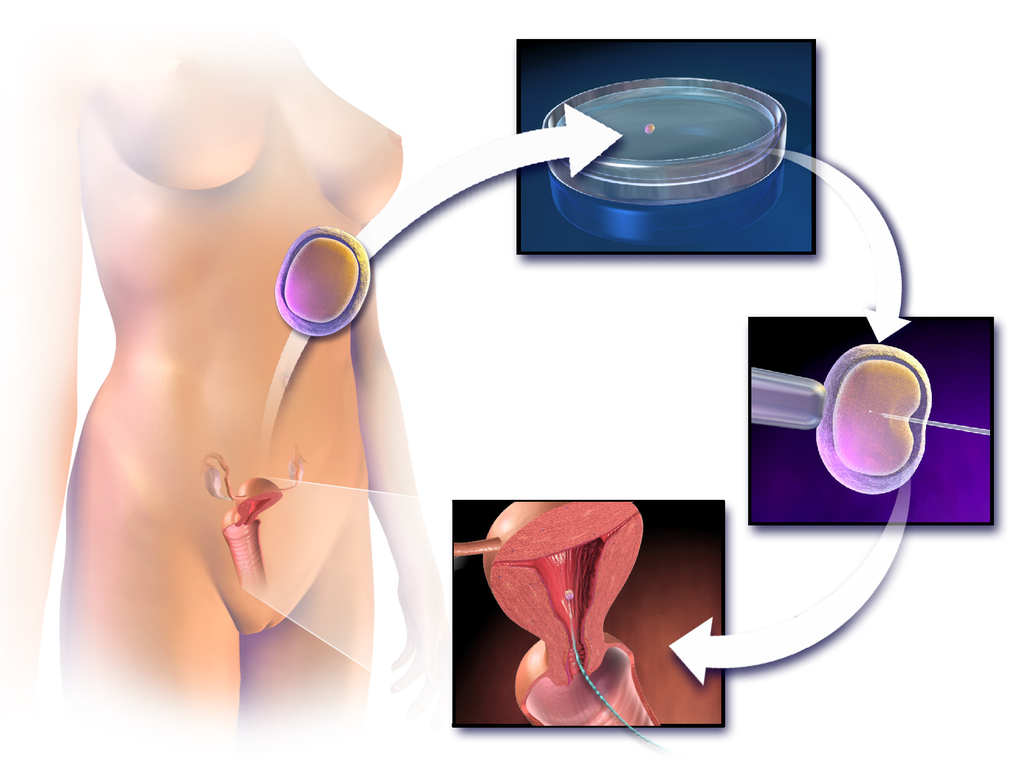
ART has about a 40% chance of leading to a live birth in women under the age of 35, but only about a 20%t chance of success in women over the age of 35. Some studies have found a higher-than-average risk of birth defects in children produced by ART procedures, but this may be due to the generally higher ages of the parent — not the technologies used.
OTHER APPROACHES
Other approaches for certain causes of infertility include the use of a surrogate mother, a gestational carrier, or sperm donation.
- A surrogate mother is a woman who agrees to become pregnant using the man’s sperm and her own egg. The child, who will be the biological offspring of the surrogate and the male partner, is given up at birth for adoption by the couple. Surrogacy might be selected by women with no eggs or unhealthy eggs. A woman who carries a mutant gene for a serious genetic disorder might choose this option to ensure that the defective gene is not passed on to the offspring.
- A gestational carrier is a woman who agrees to receive a transplanted embryo from a couple and carry it to term. The child, who will be the biological offspring of the couple, is given to the parents at birth. A gestational carrier might be used by women who have normal ovulation but no uterus, or who cannot safely carry a fetus to term because of a serious health problem (such as kidney disease or cancer).
- Sperm donation is the use of sperm from a fertile man (generally through artificial insemination) for cases in which the male partner in a couple is infertile, or in which a woman seeks to become pregnant without a male partner. A lesbian couple may use donated sperm to enable one of them to become pregnant and have a child. Sperm can be obtained from a sperm bank, which buys and stores sperm for artificial insemination, or a male friend or other individual may donate sperm to a specific woman.
SOCIAL AND ETHICAL ISSUES RELATING TO INFERTILITY
For people who have a strong desire for children of their own, infertility may lead to deep disappointment and depression. Individuals who are infertile may even feel biologically inadequate. Partners in infertile couples may argue and feel resentment toward each other, and married couples may get divorced because of infertility. Infertility treatments — especially ART procedures — are generally time-consuming and expensive. The high cost of the treatments can put them out of financial reach of many couples.
ETHICAL CONCERNS
Some people question whether the allocation of medical resources to infertility treatments is justified, and whether the resources could be better used in other ways. The status of embryos that are created in vitro and then not used for a pregnancy is another source of debate. Some people oppose their destruction on religious grounds, and couples may sometimes argue about what should be done with their extra embryos. Ethical issues are also raised by procedures that increase the chances of multiple births, because of the medical and developmental risks associated with multiple births.
INFERTILITY IN DEVELOPING COUNTRIES
Infertility is an under-appreciated problem in the poorer nations of the world, because of assumptions about overpopulation problems and high birth rates in developing countries. In fact, infertility is at least as great a problem in developing as in developed countries. High rates of health problems and inadequate health care in the poorer nations increase the risk of infertility. At the same time, infertility treatments are usually not available — or are far too expensive — for the vast majority of people who may need them. In addition, in many developing countries, the production of children is highly valued. Children may be needed for family income generation and economic security of the elderly. It is not uncommon for infertility to lead to social stigmatization, psychological problems, and abandonment by spouses.
Review
- What is infertility? How is infertility defined scientifically and medically?
- What percentage of infertility in couples is due to male infertility? What percentage is due to female infertility?
- Identify causes of and risk factors for male infertility.
- Identify causes of and risk factors for female infertility.
- How are causes of infertility in couples diagnosed?
- How is infertility treated?
- Discuss some of the social and ethical issues associated with infertility or its treatment.
- Describe two similarities between causes of male and female infertility.
- Explain the difference between males and females in terms of how age affects fertility.
14.8 CONTRACEPTION
More than half of all fertile married couples worldwide use some form of contraception. Contraception, also known as birth control, is any method or device used to prevent pregnancy. Birth control methods have been used for centuries, but safe and effective methods only became available in the 20th century.
Many different birth control methods are currently available, but they differ considerably in their effectiveness at preventing pregnancy. The effectiveness of contraception is generally expressed as the failure rate, which is the percentage of women who become pregnant using a given method during the first year of use. Virtually no one uses any method of birth control perfectly, so the failure rate with typical use is almost always higher — and often much higher — than the failure rate with perfect use. For example, with perfect use, a birth control method might have a failure rate of just 1%, whereas with typical use, the failure rate might be 25%. For comparison, there is an average one-year pregnancy rate of 85% if no contraception is used.
All methods of birth control have potential adverse effects, but their health risks are less than the health risks associated with pregnancy. Using contraception to space the children in a family is also good for the children’s health and development, as well as for the health of the mother.
TYPES OF CONTRACEPTION AND THEIR EFFECTIVENESS
Types of birth control methods include barrier methods, hormonal methods, intrauterine devices, behavioral methods, and sterilization. With the exception of sterilization, all of these methods are reversible. Examples of each type of birth control method and their failure rates with typical use are described below. Much of the information is also summarized in Figure 14.30.
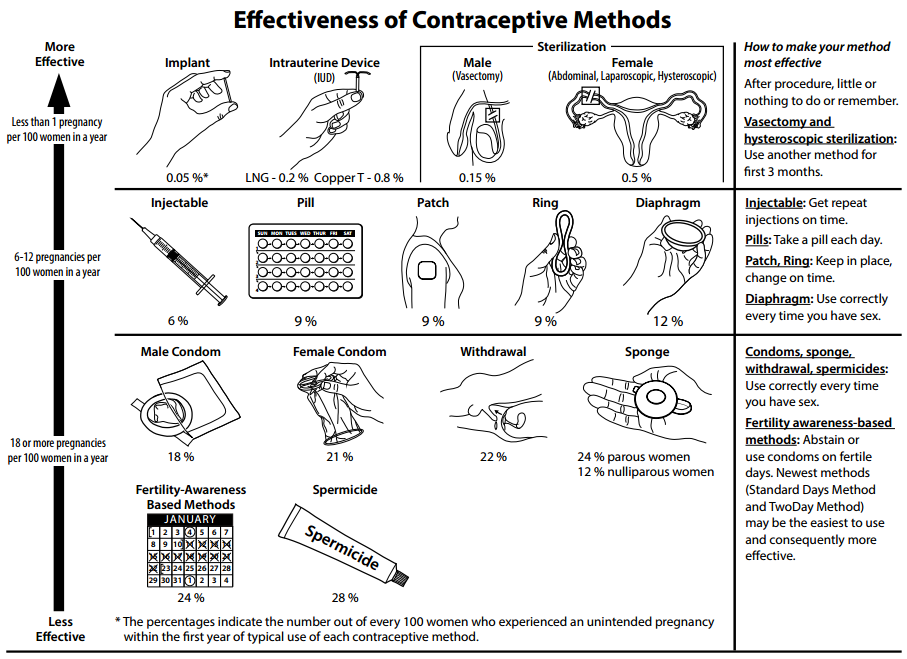
BARRIER METHODS
Barrier methods are devices that are used to physically block sperm from entering the uterus. They include condoms and diaphragms.

Condoms
Condoms are the most commonly used method of birth control globally. There are condoms for females and males, but male condoms are more widely used, less expensive, and more readily available. Both types of condoms are pictured in Figures 14.31 and 14.32. A male condom is placed on a man’s erect penis, and a female condom is placed inside a woman’s vagina. Whichever type of condom is used, it must be put in place before sexual intercourse occurs. Condoms work by physically blocking ejaculated sperm from entering the vagina of the sexual partner. With typical use, male condoms have an 18% failure rate, and female condoms have a 21% failure rate. Unlike virtually all other birth control methods, condoms also help prevent the spread of sexually transmitted infections (STIs), in addition to helping to prevent pregnancy.


Diaphragms
Diaphragms, like the one pictured in Figure 14.33, ideally prevent sperm from passing through the cervical canal and into the uterus. A diaphragm is inserted vaginally before sexual intercourse occurs and must be placed over the cervix to be effective. It is usually recommended that a diaphragm be covered with spermicide before insertion for extra protection. It is also recommended that the diaphragm be left in place for at least six hours after intercourse. The failure rate of diaphragms with typical use is about 12%, which is about half that of condoms. However, diaphragms do not help prevent the spread of STIs, and their use is also associated with an increased frequency of urinary tract infections in females.
HORMONAL METHODS
Hormonal contraception is the administration of hormones to prevent ovulation. Hormones can be taken orally in birth control pills, implanted under the skin, injected into a muscle, or received transdermally from a skin patch. Hormonal methods are currently available only for women, although hormonal contraceptives for men are being tested in clinical trials.
Birth control pills are the most common form of hormonal contraception. There are two types of pills: the combined pill (which contains both estrogen and progesterone) and the progesterone-only pill. Both types of pills inhibit ovulation and thicken cervical mucus. The failure rate of birth control pills is only about 1% or less, if used perfectly. However, the failure rate rises to about 10% with typical use, because women do not always remember to take the pill at the same time every day. The combined pill is associated with a slightly increased risk of blood clots, but a reduced risk of ovarian and endometrial cancers. The progesterone-only pill does not increase the risk of blood clots, but it may cause irregular menstrual periods. It may take a few weeks or even months for fertility to return to normal after long-term use of birth control pills.
INTRAUTERINE DEVICES
An intrauterine device (IUD) is a T-shaped or coiled plastic structure that is inserted into the uterus via the vagina and cervix that contains either copper or a hormone. You can see an IUD in the uterus in the drawing of the female reproductive system in Figure 14.34. An IUD is inserted by a physician and may be left in place for months or even years. A physician also must remove an IUD, using the strings attached to the device. The copper in copper IUDs prevents pregnancy by interfering with the movement of sperm so they cannot reach and fertilize an egg. The copper may also prevent implantation in the unlikely circumstance of a sperm managing to reach and fertilize an ovum, in which case the blastocyst/zygote would be shed during menstruation. The hormones in hormonal IUDs prevent pregnancy by thickening cervical mucus and trapping sperm. The hormones may also interfere with ovulation, so there is no egg to fertilize.
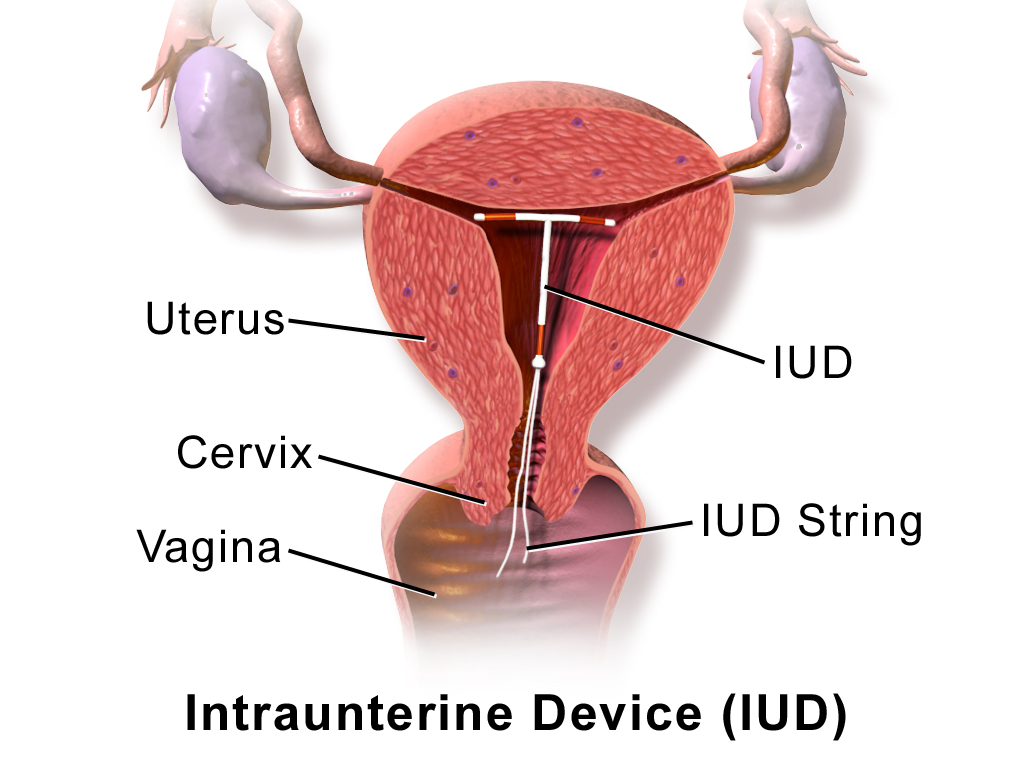
For both types of IUDs, the failure rates are <1%, and failure rates with typical use are virtually the same as failure rates with perfect use. Their effectiveness is one reason that IUDs are among the most widely used forms of reversible contraception. Once removed, even after long-term use, fertility returns to normal immediately. On the other hand, IUDs do have a risk of complications, including increased menstrual bleeding and more painful menstrual cramps. IUDs are also occasionally expelled from the uterus, and there is a slight risk of perforation of the uterus by the IUD.
BEHAVIORAL METHODS
The least effective methods of contraception are behavioral methods. They involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present. Behavioral methods include fertility awareness methods and withdrawal. Abstinence from sexual activity, or at least from vaginal intercourse, is sometimes considered a behavioral method, as well — but it is unlikely to be practiced consistently enough by most people to prevent pregnancy. Even teens who receive abstinence-only sex education do not have reduced rates of pregnancy. Abstinence is also ineffective in cases of non-consensual sex.
Fertility Awareness Methods
Fertility awareness methods involve estimating the most fertile days of the menstrual cycle and then avoiding unprotected vaginal intercourse on those days. The most fertile days are generally a few days before ovulation occurs, the day of ovulation, and another day or two after that. Unless unprotected sex occurs on those days, pregnancy is unlikely. Techniques for estimating the most fertile days include monitoring and detecting minor changes in basal body temperature or cervical secretions. This requires daily motivation and diligence, so it is not surprising that typical-use failure rates of these methods are at least 20–25%, and for some individuals may be as high as using no contraception at all (85%).
Basal body temperature is the lowest body temperature when the body is at rest (usually during sleep). It is most often estimated by a temperature measurement taken immediately upon awakening in the morning and before any physical activity has occurred. Basal body temperature normally rises after ovulation occurs, as shown in the graph below (Figure 14.35). The increase in temperature is small but consistent and may be used to determine when ovulation occurs, around which time unprotected intercourse should be avoided to prevent pregnancy. However, basal body temperature only shows when ovulation has already occurred, and it cannot predict in advance when ovulation will occur. Sperm can live for up to a week in the female reproductive tract, so determining the occurrence of ovulation only after ovulation has already happened is a major drawback of this method.
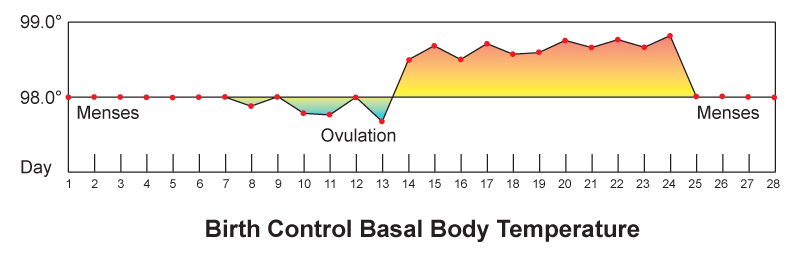
Monitoring cervical mucus has the potential for being more effective than monitoring basal body temperature, because it can predict ovulation ahead of time. As ovulation approaches, cervical secretions usually increase in amount and become thinner (which helps sperm swim through the cervical canal). By recognizing the changing characteristics of cervical mucus, a woman may be able to predict when she will ovulate. From this information, she can determine when she should avoid unprotected sex to prevent pregnancy.
Withdrawal
Withdrawal (also called coitus interruptus) is the practice of withdrawing the penis from the vagina before ejaculation ensues. The main risk of the withdrawal method is that the man may not perform the maneuver correctly or in a timely manner. Fluid typically released from the penis before ejaculation occurs may also contain some sperm. In addition, if sperm are ejaculated just outside of the vagina, there is a chance they will be able to enter the vagina and travel through the female reproductive tract to fertilize an egg. For all these reasons, the withdrawal method has a relatively high failure rate of about 22% with typical use.
STERILIZATION
The most effective contraceptive method is sterilization. In both sexes, sterilization generally involves surgical procedures that are considered irreversible. Additional surgery may be able to reverse a sterilization procedure, but there are no guarantees. Male sterilization is generally less invasive and less risky than female sterilization.
Male Sterilization
Male sterilization is usually achieved with a vasectomy. In this surgery, the vas deferens from each testis is clamped, cut, or otherwise sealed (see Figure 14.36). This prevents sperm from traveling from the epididymis to the ejaculatory ducts and being ejaculated from the penis. The same amount of semen will still be ejaculated, but it will not contain any sperm, making fertilization impossible. After a vasectomy, the testes continue to produce sperm, but the sperm are reabsorbed. It usually takes several months after a vasectomy for all remaining sperm to be ejaculated or reabsorbed. In the meantime, another method of birth control should be used.
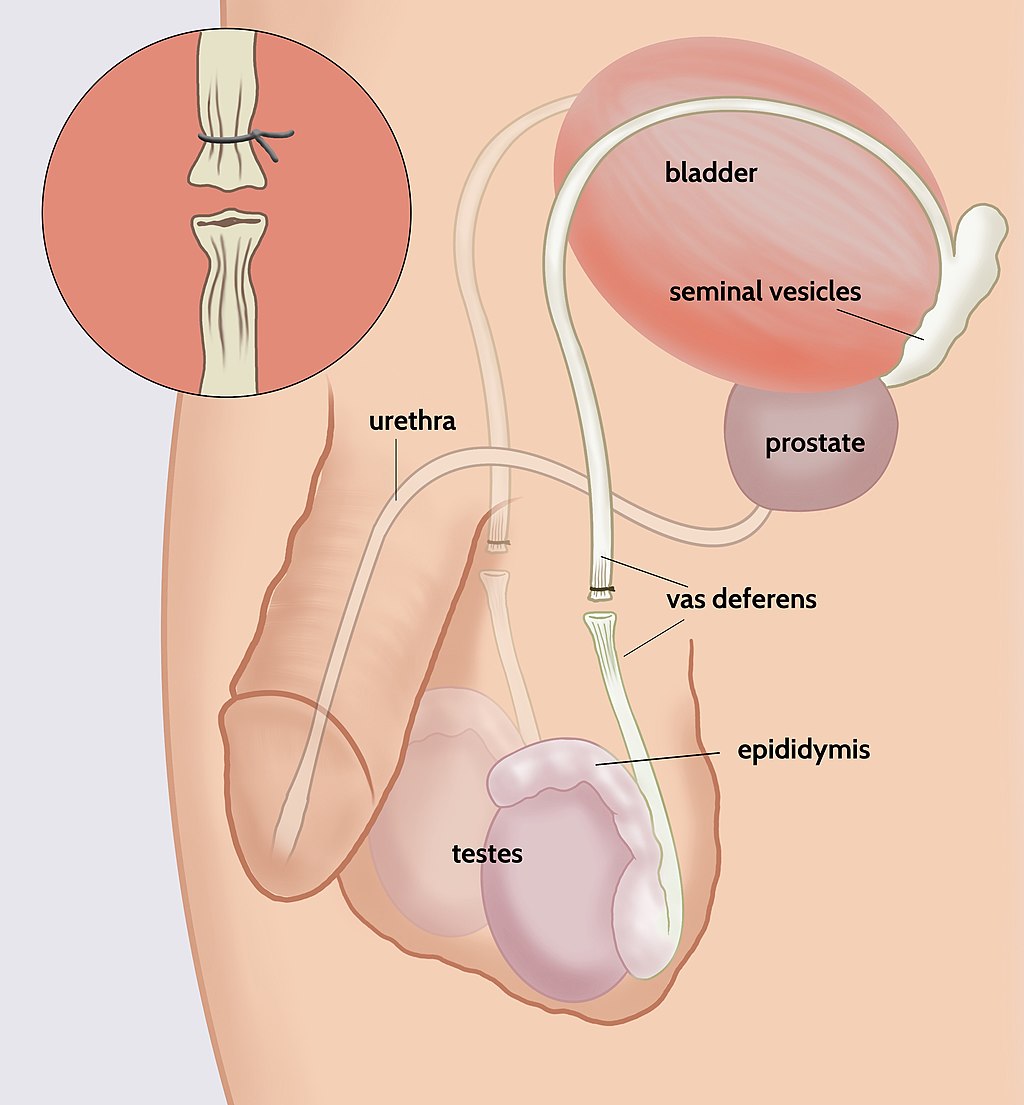
Female Sterilization
The procedure undertaken for female sterilization is usually tubal ligation. The oviducts may be tied or cut in a surgical procedure, which permanently blocks the tubes. Alternatively, tiny metal implants may be inserted into the oviducts in a nonsurgical procedure. Over time, scar tissue grows around the implants and permanently blocks the tubes. Either method stops eggs from traveling from the ovaries through the oviducts, where fertilization usually takes place.
EMERGENCY CONTRACEPTION
Emergency contraception is any form of contraception that is used after unprotected vaginal intercourse. One method is the so-called “morning-after” pill. This is essentially a high-dose birth control pill that helps prevent pregnancy by temporarily preventing ovulation. It works only if ovulation has not already occurred, and when taken within five days after unprotected sex. The sooner the pill is taken, the more likely it is to work. Another method of emergency contraception is the IUD. An IUD that is inserted up to five days after unprotected sex can prevent nearly 100% of pregnancies. It keeps sperm from reaching and fertilizing an egg or inhibits implantation if an ovum has already been fertilized. The IUD can then be left in place to prevent future pregnancies.
Review
- How is the effectiveness of contraceptive methods typically measured?
- What is an IUD?
- Discuss sterilization as a birth control method. Compare sterilization in males and females.
- What is emergency contraception? When is it used? What are two forms of emergency contraception?
- How does the thickness of cervical mucus relate to fertility? How do two methods of contraception take advantage of this relationship?
- If a newly developed method of contraception had a 35% failure rate, would you consider this to be an effective method? Explain your answer.
- Fill in the blanks:
____________________ is any method or device use to prevent pregnancy. The effectiveness of contraceptive methods is typically measured as the ________________, the percentage of women who become pregnant using a given method during the first year of use. ___________________ are the only method of birth control which also protect against sexually transmitted infections. ___________________ physically block sperm from entering the uterus. ___________________ uses hormones to prevent ovulation and typically contain ___________________ and/or estrogen. All methods of birth control are reversible, with the exception of ___________________. ____________________ is the method with the highest failure rate and involves refraining from sexual activity around the time of ovulation.
How do contraceptives work?
14.9 DISORDERS OF THE MALE REPRODUCTIVE SYSTEM
ERECTILE DYSFUNCTION
Erectile dysfunction (ED) is sexual dysfunction characterized by the regular and repeated inability of a sexually mature male to obtain or maintain an erection. It is a common disorder that affects about 40% of males, at least occasionally.
CAUSES OF ERECTILE DYSFUNCTION
The penis normally stiffens and becomes erect when the columns of spongy tissue within the shaft of the penis become engorged with blood. Anything that hampers normal blood flow to the penis may therefore interfere with its potential to fill with blood and become erect. The normal nervous control of sexual arousal or penile engorgement may also fail and lead to problems obtaining or maintaining an erection.
Specific causes of ED include both physiological and psychological causes. Physiological causes include the use of therapeutic drugs (such as antidepressants), aging, kidney failure, diseases (such as diabetes or multiple sclerosis), tobacco smoking, and treatments for other disorders (such as prostate cancer). Psychological causes are less common, but may include stress, performance anxiety, or mental disorders. The risk of ED may also be greater in men with obesity, cardiovascular disease, poor dietary habits, and overall poor physical health. Having an untreated hernia in the groin may also lead to ED.
TREATMENTS FOR ERECTILE DYSFUNCTION
Treatment of ED depends on its cause or contributing factors. For example, for tobacco smokers, smoking cessation may bring significant improvement in ED. Improving overall physical health by losing weight and exercising regularly may also be beneficial. The most common first-line treatment for ED, however, is the use of oral prescription drugs, known by brand names such as Viagra® and Cialis®. These drugs help ED by increasing blood flow to the penis. Other potential treatments include topical creams applied to the penis, injection of drugs into the penis, or the use of a vacuum pump that helps draw blood into the penis by applying negative pressure. More invasive approaches may be used as a last resort if other treatments fail. These usually involve surgery to implant inflatable tubes or rigid rods into the penis.
Ironically, the world’s most venomous spider —the Brazilian wandering spider (see Figure 14.37) — may offer a new treatment for ED. The venom of this spider is known to cause priapism in human males. Priapism is a prolonged erection that may damage the reproductive organs and lead to infertility if it continues too long. Researchers are investigating one of the components of the spider’s venom as a possible treatment for ED, if taken in minute quantities.

Epididymitis
Epididymitis is inflammation of the epididymis. The epididymis is one of the paired organs within the scrotum where sperm mature and are stored. Discomfort or pain and swelling in the scrotum are typical symptoms of epididymitis, which is a relatively common condition, especially in young men.
ACUTE VS. CHRONIC EPIDIDYMITIS
Epididymitis may be acute or chronic. Acute diseases are generally short-term conditions, whereas chronic diseases may last years — or even lifelong.
Acute Epididymitis
Acute epididymitis generally has a fairly rapid onset and is most often caused by a bacterial infection. Bacteria in the urethra can back-flow through the urinary and reproductive structures to the epididymis. In sexually active males, approximately 65% of cases of acute epididymitis are caused by sexually transmitted bacteria. Besides pain and swelling, common symptoms of acute epididymitis include redness and warmth in the scrotum, and a fever. There may also be a urethral discharge.
Chronic Epididymitis
Chronic epididymitis is epididymitis that lasts for more than three months. In some men, the condition may last for years. It may occur with or without a bacterial infection being diagnosed. Sometimes, it is associated with lower back pain that occurs after an activity that stresses the lower back, such as heavy lifting or a long period spent driving a vehicle.
TREATMENT OF EPIDIDYMITIS
If a bacterial infection is suspected, both acute and chronic epididymitis are generally treated with antibiotics. For chronic epididymitis, antibiotic treatment may be prescribed for as long as four to six weeks to ensure the complete eradication of any possible bacteria. Additional treatments often include anti-inflammatory drugs to reduce inflammation of the tissues, and painkillers to control the pain, which may be severe. Physically supporting the scrotum and applying cold compresses may also be recommended to help relieve swelling and pain.
Regardless of symptoms, treatment is important for both acute and chronic epididymitis, because major complications may occur otherwise. Untreated acute epididymitis may lead to an abscess — which is a buildup of pus — or to the infection spreading to other organs. Untreated chronic epididymitis may lead to permanent damage to the epididymis and testis, and it may even cause infertility.
MALE REPRODUCTIVE CANCERS

Why does the airplane in Figure 14.33 have a huge mustache on its “face”? The mustache is a symbol of “Movember.” This is an international campaign to raise awareness of prostate cancer, as well as money to fund prostate cancer research.
PROSTATE CANCER
The prostate gland is an organ located in the male pelvis. The urethra passes through the prostate gland after it leaves the bladder and before it reaches the penis. The function of the prostate is to secrete zinc and other substances into semen during an ejaculation. In Canada, prostate cancer is the most common type of cancer in men, and the second leading cause of male cancer death. About 1 in 9 Canadian men will be diagnosed with prostate cancer. Prostate cancer occurs at higher rates in rich nations like Canada and the United States, but the rates are increasing everywhere.
How Prostate Cancer Occurs
Prostate cancer occurs when glandular cells of the prostate mutate into tumor cells. Eventually, the tumor, if undetected, may invade nearby structures, such as the seminal vesicles. Tumor cells may also metastasize and travel in the bloodstream or lymphatic system to organs elsewhere in the body. Prostate cancer most commonly metastasizes to the bones, lymph nodes, rectum, or lower urinary tract organs.
Symptoms of Prostate Cancer
Early in the course of prostate cancer, there may be no symptoms. When symptoms do occur, they mainly involve urination, because the urethra passes through the prostate gland. The symptoms typically include frequent urination, difficulty starting and maintaining a steady stream of urine, blood in the urine, and painful urination. Prostate cancer may also cause problems with sexual function, such as difficulty achieving erection or painful ejaculation.
Risk Factors for Prostate Cancer
Some factors that increase the risk of prostate cancer can be changed, and others cannot.
- Risk factors that can be changed include a diet high in meat, a sedentary lifestyle, obesity, and high blood pressure.
- Risk factors that cannot be changed include older age, a family history of prostate cancer, and African ancestry. Family history is an important risk factor, so genes are clearly involved. Many different genes have been implicated.
Diagnosing Prostate Cancer
The only definitive test to confirm a diagnosis of prostate cancer is a biopsy. In this procedure, a small piece of the prostate gland is surgically removed and then examined microscopically. A biopsy is done only after less invasive tests have found evidence that a patient may have prostate cancer.
A routine exam by a doctor may find a lump on the prostate, which might be followed by a blood test that detects an elevated level of prostate-specific antigen (PSA). PSA is a protein secreted by the prostate that normally circulates in the blood. Higher-than-normal levels of PSA can be caused by prostate cancer, but they may also have other causes. Ultrasound or magnetic resonance imaging (MRI) might also be undertaken to provide images of the prostate gland and additional information about the cancer.
Treatment of Prostate Cancer
The average age at which men are diagnosed with prostate cancer is 70 years. Prostate cancer typically is such a slow-growing cancer that elderly patients may not require treatment. Instead, the patients are watched carefully over the subsequent years to make sure the cancer isn’t growing and posing an immediate threat — an approach that is called active surveillance. It is used for at least 50% of patients who are expected to die from other causes before their prostate cancer causes symptoms.
Treatment of younger patients — or those with more aggressively growing tumors — may include surgery to remove the prostate, chemotherapy, and/or radiation therapy (such as brachytherapy, see Figure 14.39). All of these treatment options can have significant side effects, such as erectile dysfunction or urinary incontinence. Patients should learn the risks and benefits of the different treatments, and discuss them with their healthcare provider to decide on the best treatment options for their particular case.
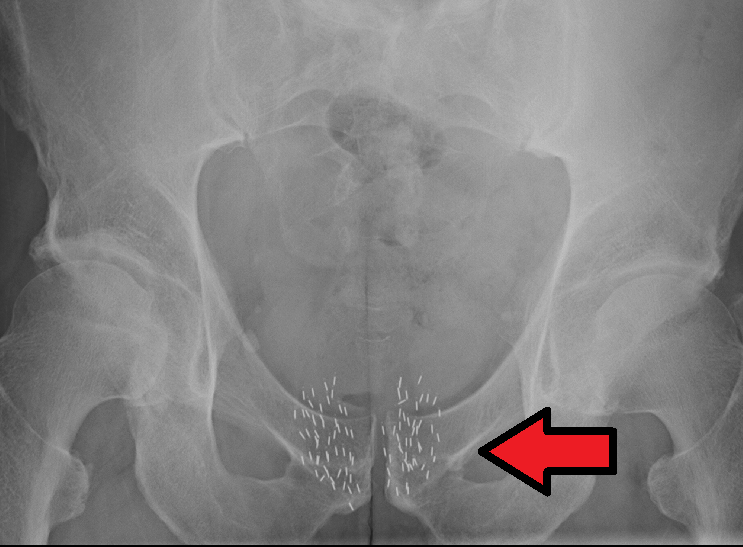
TESTICULAR CANCER
The reproductive cancer that most commonly affects young men is testicular cancer. The testes are the paired reproductive organs in the scrotum that produce sperm and secrete testosterone. Although testicular cancer is rare, it is one of the few cancers that is more common in younger than older people. In fact, cancer of the testis is the most common cancer in males between the ages of 20 and 39 years. The risk of testicular cancer is about four to five times greater in men of European than African ancestry. The cause of this difference is unknown.
Signs and Symptoms of Testicular Cancer
One of the first signs of testicular cancer is often a lump or swelling in one of the two testes. The lump may or may not be painful. If pain is present, it may occur as a sharp pain or a dull ache in the lower abdomen or scrotum. Some men with testicular cancer report a feeling of heaviness in the scrotum. Testicular cancer does not commonly spread beyond the testis, but if it does, it most often spreads to the lungs, where it may cause shortness of breath or a cough.
Diagnosis of Testicular Cancer
The main way that testicular cancer is diagnosed is by detection of a lump in the testis. This is likely followed by further diagnostic tests. An ultrasound may be done to determine the exact location, size, and characteristics of the lump. Blood tests may be done to identify and measure tumor-marker proteins in the blood that are specific to testicular cancer. CT scans may also be done to determine whether the disease has spread beyond the testis. However, unlike the case with prostate cancer, a biopsy is not recommended, because it increases the risk of cancer cells spreading into the scrotum.
Treatment of Testicular Cancer
Testicular cancer has one of the highest cure rates of all cancers; it is estimated that 1 in every 250 men will develop this cancer in their lifetime. Three basic types of treatment for testicular cancer are surgery, radiation therapy, and/or chemotherapy. Generally, the initial treatment is surgery to remove the affected testis. If the cancer is caught at an early stage, the surgery is likely to cure the cancer and has nearly a 100% five-year survival rate. When just one testis is removed, the remaining testis (if healthy) is adequate to maintain fertility, hormone production, and other normal male functions. Radiation therapy and/or chemotherapy may follow surgery to kill any tumor cells that might exist outside the affected testis, even when there is no indication that the cancer has spread. In many cases, however, surgery is followed by surveillance instead of additional treatments.
Review
- Identify some of the underlying causes of erectile dysfunction. Discuss types of treatment for erectile dysfunction.
- Identify possible treatments for epididymitis. Why is treatment important, even when there are no symptoms?
- What are some of the symptoms of prostate cancer? List risk factors for prostate cancer. How is prostate cancer detected?
- In many cases, treatment for prostate cancer is unnecessary. Why? When is treatment necessary, and what are treatment options?
- Testicular cancer is generally rare, but it is the most common cancer in one age group. What age group is it?
- Identify possible signs and symptoms of testicular cancer. How can testicular cancer be diagnosed? Describe how testicular cancer is typically treated.
14.10 DISORDERS OF THE FEMALE REPRODUCTIVE SYSTEM

VACCINATING AGAINST CANCER
Can a vaccine prevent cancer? In the case of cervical cancer, it can. Cervical cancer is one of three disorders of the female reproductive system described in detail in this concept. Of the three, only cervical cancer can be prevented with a vaccine.
CERVICAL CANCER
Cervical cancer occurs when cells of the cervix (neck of the uterus) grow abnormally and develop the ability to invade nearby tissues or spread to other parts of the body, such as the abdomen or lungs.
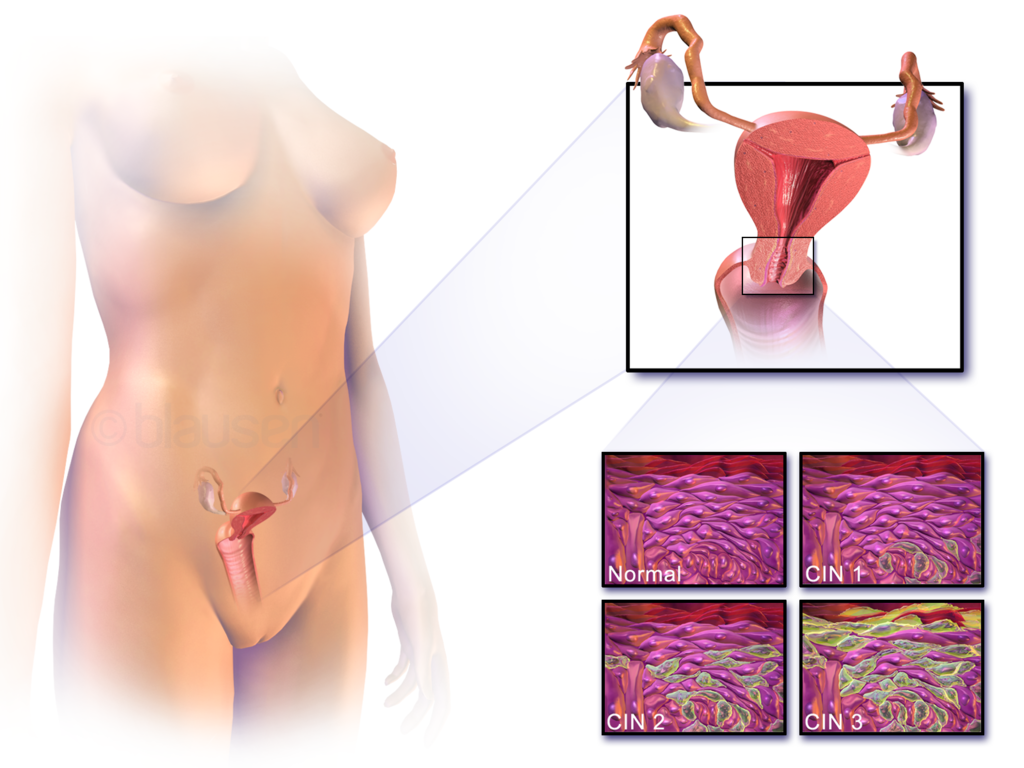
CERVICAL CANCER PREVALENCE AND DEATH RATES
Worldwide, cervical cancer is the second most common type of cancer in females (after breast cancer) and the fourth-most common cause of cancer death in females. In Canada and other high-income nations, the widespread use of cervical cancer screening has detected many cases of precancerous cervical changes and has dramatically reduced rates of cervical cancer deaths. About 75% of cervical cancer cases occur in developing countries, where routine screening is less likely because of cost and other factors. Cervical cancer is also the most common cause of cancer death in low-income countries.
SYMPTOMS OF CERVICAL CANCER
Early in the development of cervical cancer, there are typically no symptoms. As the disease progresses, however, symptoms are likely to occur. The symptoms may include abnormal vaginal bleeding, pelvic pain, or pain during sexual intercourse. Unfortunately, by the time symptoms start to occur, cervical cancer has typically progressed to a stage at which treatment is less likely to be successful.
CERVICAL CANCER CAUSES AND RISK FACTORS
More than 90 per cent of cases of cervical cancer are caused at least in part by human papillomavirus (HPV), which is a sexually transmitted virus that also causes genital warts. Figure 14.42 shows how HPV infection can cause cervical cancer by interfering with a normal cell division checkpoint. When HPV is not present, cervical cells containing mutations are not allowed to divide, so the cervix remains healthy. When HPV is present, however, cervical cells with mutations may be allowed to divide, leading to uncontrolled growth of mutated cells and the formation of a tumor.
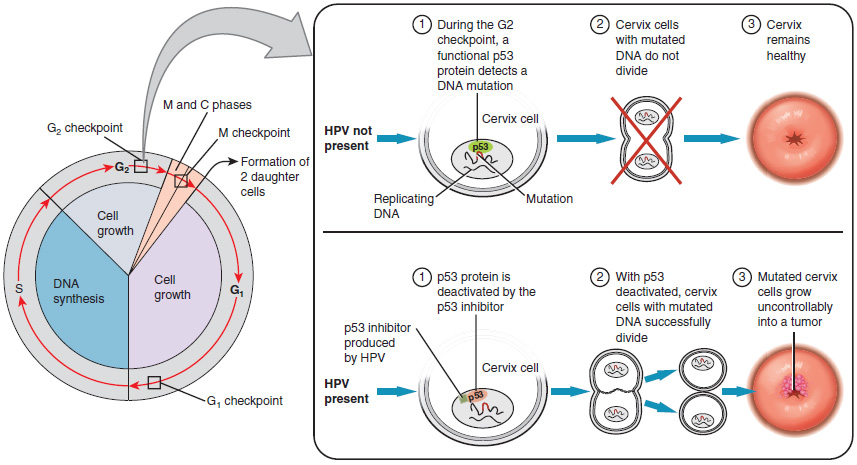
Other risk factors for cervical cancer include smoking, a weakened immune system (for example, due to HIV infection), use of birth control pills, becoming sexually active at a young age, and having many sexual partners. However, these risk factors are less important than HPV infection. Instead, the risk factors are more likely to increase the risk of cervical cancer in females who are already infected with HPV. For example, among HPV-infected women, current and former smokers have roughly two to three times the incidence of cervical cancer as non-smokers. Passive smoking, or secondhand smoke, is also associated with an increased risk of cervical cancer, but to a lesser extent.
DIAGNOSIS OF CERVICAL CANCER
Diagnosis of cervical cancer is typically made by looking for microscopic abnormal cervical cells in a smear of cells scraped off the cervix. This is called a Pap smear. If cancerous cells are detected or suspected in the smear, this test is usually followed up with a biopsy to confirm the Pap smear results. Medical imaging (by CT scan or MRI, for example) is also likely to be done to provide more information, such as whether the cancer has spread.
PREVENTION OF CERVICAL CANCER
It is now possible to prevent HPV infection with a vaccine. The first HPV vaccine was approved by the U.S. Food and Drug Administration in 2006. The vaccine protects against the strains of HPV that have the greatest risk of causing cervical cancer. It is thought that widespread use of the vaccine will prevent up to 90% of cervical cancer cases. Current recommendations are for females to be given the vaccine between the ages of nine and 26. (Boys should be vaccinated against HPV, as well, because the virus may also cause cancer of the penis and certain other male cancers.) The vaccine is effective only if it is given before HPV infection has occurred. Using condoms during sexual intercourse can also help prevent HPV infection and cervical cancer, in addition to preventing pregnancy and sexually transmitted infections (such as HIV).
Even in women who have received the HPV vaccine, there is still a small risk of developing cervical cancer. Therefore, it is recommended that women continue to be examined with regular Pap smears.
TREATMENT OF CERVICAL CANCER
Treatment of cervical cancer generally depends on the stage at which the cancer is diagnosed, but it is likely to include some combination of surgery, radiation therapy, and/or chemotherapy. Outcomes of treatment depend largely on how early the cancer is diagnosed and treated. For surgery to cure cervical cancer, the entire tumor must be removed with no cancerous cells found at the margins of the removed tissue on microscopic examination. If cancer is found and treated very early when it is still in the microscopic stage, the five-year survival rate is virtually 100%.
VAGINITIS
Vaginitis is inflammation of the vagina — and sometimes the vulva, as well. Symptoms may include a discharge that is yellow, gray, or green; itching; pain; and a burning sensation. There may also be a foul vaginal odor and pain or irritation with sexual intercourse.
CAUSES OF VAGINITIS
About 90% of cases of vaginitis are caused by infection with microorganisms. Most commonly, vaginal infections are caused by the yeast Candida albicans (see Figure 14.43). Such infections are referred to as vaginal candidiasisor more commonly as a yeast infection. Candida albicans is one of the most common opportunistic infections in the world and can affect not only the vagina, but any of the mucus membranes and skin. Other possible causes of vaginal infections include bacteria, especially Gardnerella vaginalis, and some single-celled parasites, notably the protist parasite Trichomonas vaginalis, which is usually transmitted through vaginal intercourse. The risk of vaginal infections may be greater in women who wear tight clothing, are taking antibiotics for another condition, use birth control pills, or have improper hygiene. Poor hygiene allows organisms that are normally present in the stool (such as yeast) to contaminate the vagina.
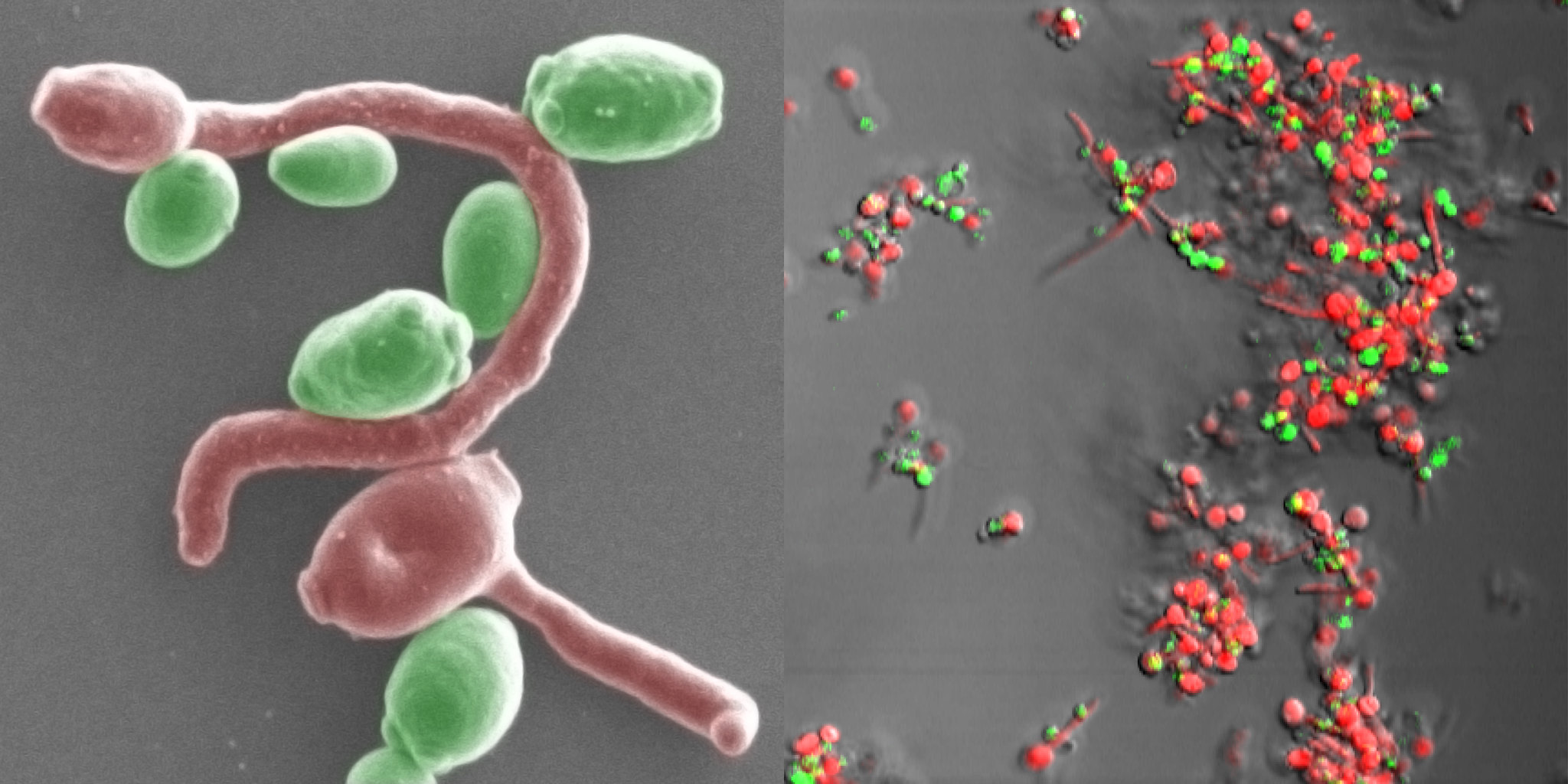
Most of the remaining cases of vaginitis are due to irritation by — or allergic reactions to — various products. These irritants may include condoms, spermicides, soaps, douches, lubricants, and even semen. Using tampons or soaking in hot tubs may be additional causes of this type of vaginitis.
DIAGNOSIS OF VAGINITIS
Diagnosis of vaginitis typically begins with symptoms reported by the patient. This may be followed by a microscopic examination or culture of the vaginal discharge in order to identify the specific cause. The color, consistency, acidity, and other characteristics of the discharge may be predictive of the causative agent. For example, infection with Candida albicans may cause a cottage cheese-like discharge with a low pH, whereas infection with Gardnerella vaginalis may cause a discharge with a fish-like odor and a high pH.
PREVENTION OF VAGINITIS
Prevention of vaginitis includes wearing loose cotton underwear that helps keep the vulva dry. Yeasts and bacteria that may cause vaginitis tend to grow best in a moist environment. It is also important to avoid the use of perfumed soaps, personal hygiene sprays, and douches, all of which may upset the normal pH and bacterial balance in the vagina. To help avoid vaginitis caused by infection with Trichomonas vaginalis, the use of condoms during sexual intercourse is advised.
TREATMENT OF VAGINITIS
The appropriate treatment of vaginitis depends on the cause. In many cases of vaginitis, there is more than one cause, and all of the causes must be treated to ensure a cure.
- Yeast infections of the vagina are typically treated with topical anti-fungal medications, which are available over the counter. The medications may be in the form of tablets or creams that are inserted into the vagina. Depending on the particular medication used, treatment may involve one, three, or seven days of applications.
- Bacterial infections of the vagina are usually treated with antibiotics. These may be taken orally as pills, or applied topically to the vagina in creams.
- Trichomonas vaginalis infections of the vagina are generally treated with a single dose of an oral antibiotic. Sexual partners should be treated at the same time, and intercourse should be avoided for at least a week until both partners have completed treatment, and have been followed-up by a physician.
ENDOMETRIOSIS
Endometriosis is a disease in which endometrial tissue, which normally grows inside the uterus, grows outside it, as shown in Figure 14.44. Most often, the endometrial tissue grows around the ovaries, Fallopian tubes, and uterus. In rare instances, the tissue may grow elsewhere in the body. The areas of endometriosis typically bleed each month during the menstrual period, and this often results in inflammation, pain, and scarring. An estimated six to ten per cent of women are believed to have endometriosis. It is most common in women during their thirties and forties, and only rarely occurs before menarche or after menopause.
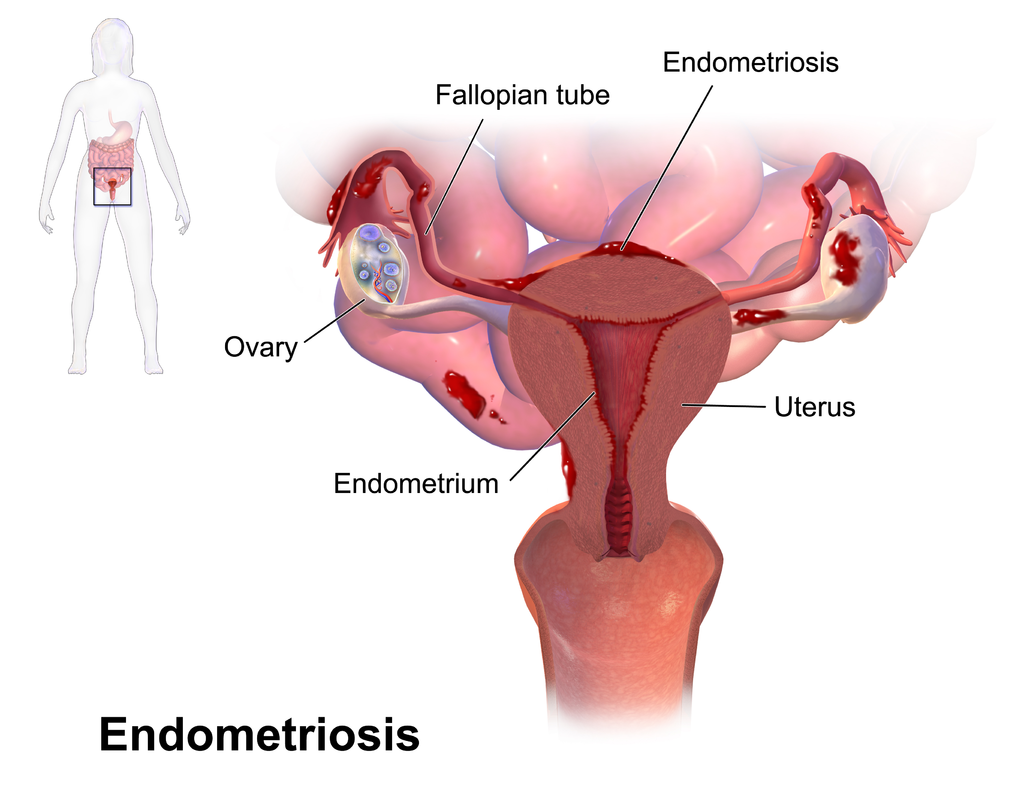
SIGNS AND SYMPTOMS OF ENDOMETRIOSIS
The main symptom of endometriosis is pelvic pain, which may range from mild to severe. There appears to be little or no relationship between the amount of endometrial tissue growing outside the uterus and the severity of the pain. For many women with the disease, the pain occurs mainly during menstruation. However, nearly half of those affected have chronic pelvic pain. The pain of endometriosis may be caused by bleeding in the pelvis, which triggers inflammation. Pain can also occur from internal scar tissue that binds internal organs to each other.
Another problem often associated with endometriosis is infertility, or the inability to conceive or bear children. Among women with endometriosis, up to half may experience infertility. Infertility can be related to scar formation or to anatomical distortions due to the abnormal endometrial tissue. Other possible symptoms of endometriosis may include diarrhea or constipation, chronic fatigue, nausea and vomiting, headaches, and heavy or irregular menstrual bleeding.
CAUSES OF ENDOMETRIOSIS
The causes of endometriosis are not known for certain, but several risk factors have been identified, including a family history of endometriosis. Daughters or sisters of women with endometriosis have about six times the normal risk of developing the disease themselves. It has been suggested that endometriosis results from mutations in several genes. It is likely that endometriosis is multifactorial, involving the interplay of several factors.
At the physiological level, the predominant idea for how endometriosis comes about is retrograde menstruation. This happens when some of the endometrial debris from a woman’s menstrual flow exits the uterus through the oviducts, rather than through the vagina. The debris then attaches itself to the outside of organs in the abdominal cavity, or to the lining of the abdominal cavity itself. Retrograde menstruation, however, does not explain all cases of endometriosis, so other factors are apparently involved. Suggestions include environmental toxins and autoimmune responses.
DIAGNOSIS OF ENDOMETRIOSIS
Diagnosis of endometriosis is usually based on self-reported symptoms and a physical examination by a doctor, often combined with medical imaging, such as ultrasonography. The only way to definitively diagnose endometriosis, however, is through visual inspection of the endometrial tissue. This can be done with a surgical procedure called laparoscopy, shown in Figure 14.45, in which a tiny camera is inserted into the abdomen through a small incision. The camera allows the physician to visually inspect the area where endometrial tissue is suspected.
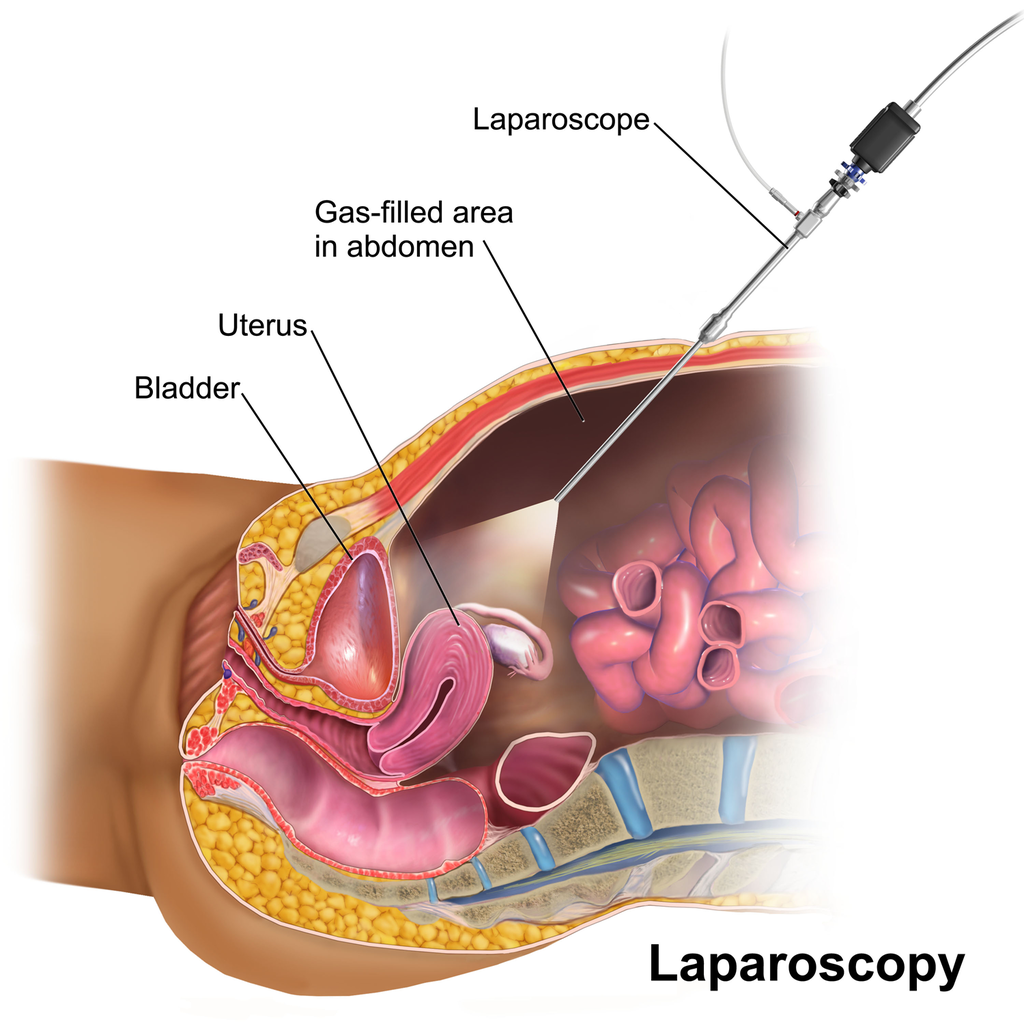
TREATMENT OF ENDOMETRIOSIS
The most common treatments for endometriosis are medications to control the pain, and surgery to remove the abnormal tissue. Frequently used pain medications are non-steroidal inflammatory drugs (NSAIDS), such as naproxen. Opiates may be used in cases of severe pain. Laparoscopy can be used to surgically treat endometriosis, as well as to diagnose the condition. In this type of surgery, an additional small incision is made to insert instruments that the surgeon can manipulate externally in order to burn (cauterize) or cut away the endometrial growths. In younger women who want to have children, surgery is conservative to keep the reproductive organs intact and functional. However, with conservative surgery, endometriosis recurs in 20–40% of cases within five years of the surgery. In older women who have completed childbearing, hysterectomy may be undertaken to remove all or part of the internal reproductive organs. This is the only procedure that is likely to cure endometriosis and prevent relapses.
FEATURE: MY HUMAN BODY
A Pap smear is a method of cervical cancer screening used to detect potentially pre-cancerous and cancerous cells in the cervix. It is the most widely used screening test for this type of cancer, and it is very effective. The test may also detect vaginal infections and abnormal endometrial cells, but it is not designed for these purposes.
According to HealthLink BC, females should start receiving routine Pap smears by age 25. Because most cases of cervical cancer are caused by infection with human papillomavirus (HPV), which is a sexually transmitted infection, there is little or no benefit to screening people who have not had sexual contact. Starting at age 25, general guidelines are for Pap smears to be repeated every three years until age 69. Screening may be discontinued after 69 years of age, if the last three Pap smears were normal. If a woman has a complete hysterectomy, she no longer has a cervix and there is no need for further Pap smears. On the other hand, if a woman has had a history of abnormal Pap smears or cancer, she will likely be screened more frequently. Pap smears can be done safely during the first several months of pregnancy and resumed about three months after childbirth. Generally, better results are obtained if Pap smears are not done during menstruation.
If you’ve never had a Pap smear, knowing what to expect may help prepare you for the procedure. The patient lies on the examining table with her feet in “stirrups” to hold the legs up and apart. An instrument called a speculum is inserted into the vagina to hold back the vaginal walls and give access to the cervix. A tiny amount of tissue is brushed off the cervix and smeared onto a microscope slide. The speculum is then removed, and the procedure is over. The slide is later examined under a microscope for abnormal cells. Some women experience light spotting or mild diarrhea after a Pap smear, but most have no lasting effects.
Pap smears are uncomfortable and may be somewhat painful for some women. If you experience pain during a Pap smear, tell your health care provider. Many steps can be taken to minimize the pain, which might include using a smaller speculum, using warm instruments and a lubricant, and applying a topical anesthetic such as lidocaine to the cervix before obtaining the smear. Any pain is generally very brief, and the potential reward is worth it. Pap tests are estimated to reduce up to 80% of cervical cancer deaths. One of the lives saved could be your own.
Review
- What is cervical cancer? Worldwide, how prevalent is it, and how does it rank as a cause of cancer deaths?
- Identify symptoms of cervical cancer. What are causes of — and risk factors for — cervical cancer?
- What roles can Pap smears and HPV vaccines play in preventing cervical cancer cases and cervical cancer deaths?
- How is cervical cancer treated?
- Define vaginitis and identify its symptoms.
- What are some of the causes of vaginitis? Which cause is responsible for most of the cases?
- How is vaginitis diagnosed and treated?
- What is endometriosis, and what are its symptoms?
- Discuss possible causes of endometriosis.
- How is endometriosis treated? Which treatment is most likely to prevent recurrence of the disorder?
- In the case of infection with Trichomonas vaginalis, why is the woman’s sexual partner usually treated at the same time?
What is HPV and how can you protect yourself from it? – Emma Bryce, TED-Ed, 2019.
14.11 CASE STUDY: TRYING TO CONCEIVE
Alicia, 28, and Victor, 30, have been married for three years. A year ago, they decided they wanted to have a baby, and they stopped using birth control. At first, they did not pay attention to the timing of their sexual activity in relation to Alicia’s menstrual cycle, but after six months passed without Alicia becoming pregnant, they decided to try to maximize their efforts.
They knew that in order for a woman to become pregnant, the man’s sperm must encounter the woman’s egg, which is typically released once a month through a process called ovulation. They also had heard that for the average woman, ovulation occurs around day 14 of the menstrual cycle. To maximize their chances of conception, they tried to have sexual intercourse on day 14 of Alicia’s menstrual cycle each month.
After several months of trying this method, Alicia is still not pregnant. She is concerned that she may not be ovulating on a regular basis, because her menstrual cycles are irregular and often longer than the average 28 days. Victor is also concerned about his own fertility. He had some injuries to his testicles (testes) when he was younger, and wonders if that may have caused a problem with his sperm.
Alicia calls her doctor for advice. Dr. Bashir recommends that she try taking her temperature each morning before she gets out of bed. This temperature is called basal body temperature (BBT), and recording BBT throughout a woman’s menstrual cycle can sometimes help identify if and when she is ovulating. Additionally, Dr. Bashir recommends she try using a home ovulation predictor kit, which predicts ovulation by measuring the level of luteinizing hormone (LH) in urine. In the meantime, Dr. Bashir sets up an appointment for Victor to give a semen sample, so that his sperm may be examined with a microscope.
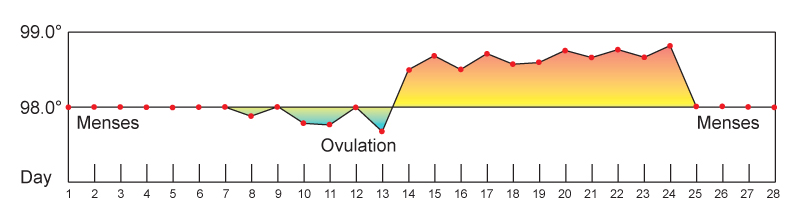
Figure 14.46 Monitoring body temperature before getting out of bed in the morning can often help tell if and when a woman is ovulating because a women’s body temperature fluctuates during a monthly cycle. Usually, a special highly sensitive thermometer is used.
The woman in Figure 14.47 is holding a home pregnancy test. The two pink lines in the middle are the type of result that Alicia and Victor are desperately hoping to see themselves one day — a positive pregnancy test. In the beginning of the chapter you learned that Alicia and Victor have been actively trying to get pregnant for a year, which, as you now know, is the time frame necessary for infertility to be diagnosed.

Figure 14.47 Success!
Alicia and Victor tried having sexual intercourse on day 14 of her menstrual cycle to optimize their chances of having his sperm meet her ovum. Why might this not be successful, even if they do not have fertility problems? Although the average menstrual cycle is 28 days, with ovulation occurring around day 14, many women vary widely from these averages (either consistently or variably) from month to month. Recall, for example, that menstrual cycles may vary from 21 to 45 days in length, and a woman’s cycle is considered to be regular if it varies within as many as eight days from shortest to longest cycle. This variability means that ovulation often does not occur on or around day 14, particularly if the woman has significantly shorter, longer, or irregular cycles — like Alicia does. Therefore, by aiming for day 14 without knowing when Alicia is actually ovulating, they may not be successful in helping Victor’s sperm encounter Alicia’s egg.
Lack of ovulation entirely can also cause variability in menstrual cycle length. As you have learned, the regulation of the menstrual cycle depends on an interplay of hormones from the pituitary gland and ovaries, including FSH and LH from the pituitary and estrogen and progesterone from the ovary — specifically from the follicle which surrounds the maturing egg and becomes the corpus luteum after ovulation. Shifts in these hormones and processes can affect ovulation and menstrual cycle length. This is why Alicia was concerned about her long and irregular menstrual cycles. If they are a sign that she is not ovulating, that could be the reason why she is having trouble getting pregnant.
In order to get a better idea of whether Alicia is ovulating, Dr. Bashir recommended that she take her basal body temperature (BBT) each morning before getting out of bed, and track it throughout her menstrual cycle. As you have learned, BBT typically rises slightly and stays high after ovulation. While tracking BBT is not a particularly effective form of contraception, since the temperature rise occurs only after ovulation, it can be a good way to see whether a woman is ovulating at all. Although not every woman will see a clear shift in BBT after ovulation, it is a relatively easy way to start assessing a woman’s fertility and is used as part of a more comprehensive fertility assessment by some physicians.
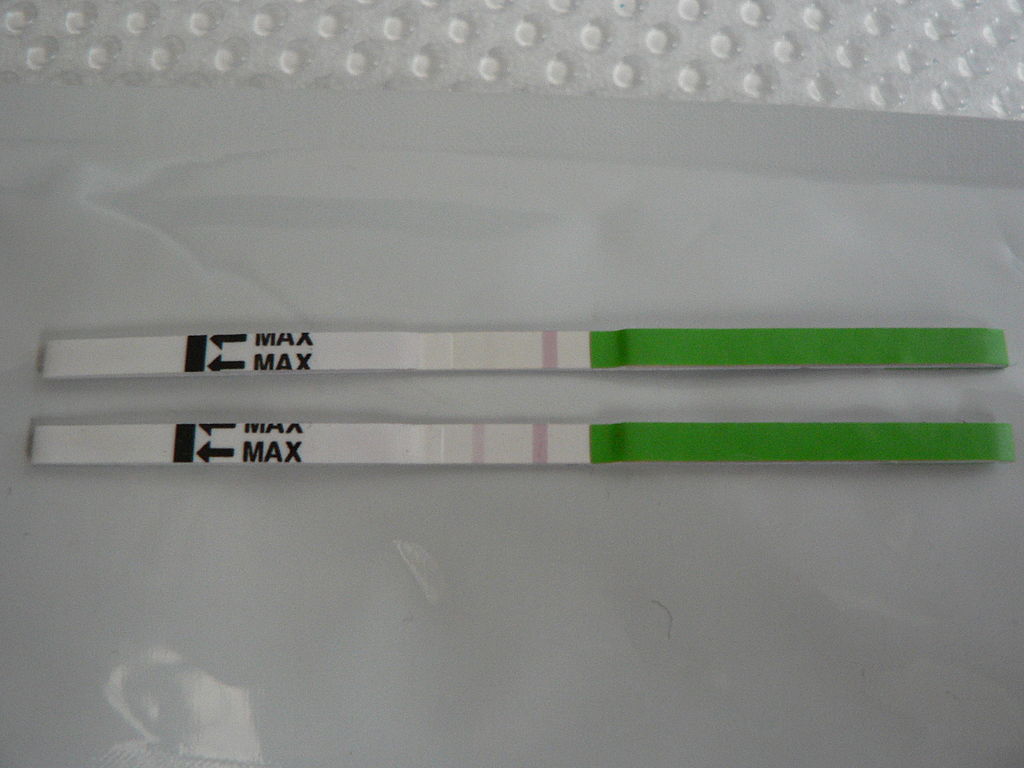
Dr. Bashir also recommended that Alicia use a home ovulation predictor kit. This is another relatively cheap and easy way to assess ovulation. Most ovulation predictor kits work by detecting the hormone LH in urine using test strips, like the ones shown in Figure 14.48. Why can this predict ovulation? Think about what you have learned about how ovulation is triggered. Rising levels of estrogen from the maturing follicle in the ovary causes a surge in the level of LH secreted from the pituitary gland, which triggers ovulation. This surge in LH can be detected by the home kit, which compares the level of LH in a woman’s urine to that of a control on the strip. After the LH surge is detected, ovulation will typically occur within one to two days.
By tracking her BBT and using the ovulation predictor kit, Alicia has learned that she is most likely ovulating, but not in every cycle, and sometimes she ovulates much later than day 14. Because frequent anovulatory cycles can be a sign of an underlying hormonal disorder, such as polycystic ovary syndrome (PCOS) or problems with the pituitary or other glands that regulate the reproductive system, Dr. Bashir orders blood tests for Alicia and sets up an appointment for a physical exam.
However, because Alicia is sometimes ovulating, the problem may not lie solely with her. Recall that infertility occurs in similar proportions in men and women, and can be due to problems in both partners. This is why it is generally recommended that both partners get assessed for fertility issues when they are having trouble getting pregnant after a year of trying.
Therefore, Victor proceeds with the semen analysis that Dr. Bashir recommended. In this process, the man provides a semen sample by ejaculating into a cup or special condom, and the semen is then examined under a microscope. The semen is then checked for sperm number, shape, and motility. Sperm with an abnormal shape or trouble moving will likely have trouble reaching and fertilizing an egg. A low number of sperm will also reduce the chances of conception. In this way, semen analysis can provide insight into the possible underlying causes of infertility. For instance, a low sperm count could indicate problems in sperm production or a blockage in the male reproductive tract that is preventing sperm from being emitted from the penis. Further testing would have to be done to distinguish between these two possible causes.
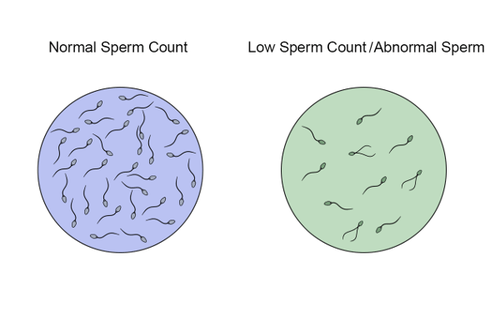
Victor had been worried that past injuries to his testes may have affected his fertility. You may remember the testes are where sperm are produced, and because they are external to the body, they are vulnerable to injury. In addition to physical damage to the testes and other parts of the male reproductive tract, a testicular injury could potentially cause the creation of antibodies against a man’s own sperm. As you have learned, Sertoli cells lining the seminiferous tubules are tightly packed so that the developing sperm are normally well-separated from the body’s immune system. However, in the case of an injury, this barrier can be breached, which can cause the creation of antisperm antibodies. These antibodies can hamper fertility by killing the sperm, or otherwise interfering with their ability to move or fertilize an egg. When infertility is due to such antibodies, it is called “immune infertility.”
Victor’s semen analysis shows that he has normal numbers of healthy sperm. Dr. Bashir recommends that while they investigate whether Alicia has an underlying medical issue, she continue to track her BBT and use ovulation predictor kits to try to pinpoint when she is ovulating. She recommends that once Alicia sees an LH surge, the couple try to have intercourse within three days to maximize their chances of conception. If Alicia is found to have a medical problem that is inhibiting ovulation, depending on what it is, they may either address the problem directly, or she can take medication that stimulates ovulation, such as clomiphene citrate (often sold under the brand name Clomid). This medication works by increasing the amount of FSH secreted by the pituitary.
Fortunately, tracking ovulation at home and timing intercourse appropriately was all Alicia and Victor needed to do to finally get pregnant! After their experience, they, like you, now have a much deeper understanding of the intricacies of the reproductive system and the complex biology that is involved in the making of a new human organism.
Attributions
This chapter is composed of text taken from of the following sources:
Clark, M. A., Douglas, M., & Choi, J. (2018, March 28). Hormonal control of human reproduction. In Human Biology (Updated April 26, 2024). Rice University. Licensed under Creative Commons Attribution 4.0 International License. Retrieved from [43.4 Hormonal Control of Human Reproduction – Biology 2e | OpenStax]
Cushwa, W., & Senior Contributors. (2015). Human biology. OpenStax CNX. [CC BY 4.0 license]. [Retrieved from Human Biology : Willy Cushwa : Free Download, Borrow, and Streaming : Internet Archive]
Lumen Learning. (n.d.). The ovarian cycle, the menstrual cycle, and menopause. In Biology 2e. Retrieved August 6, 2024, from https://courses.lumenlearning.com/wm-biology2/chapter/the-ovarian-cycle-the-menstrual-cycle-and-menopause/
Miller, C. (2020). Human biology: Human anatomy and physiology. Thompson Rivers University. [CC BY NC]. Retrieved from [Human Biology – Simple Book Publishing (tru.ca)]

